Introduction
Sepsis is the primary cause of death from infection. Although wide-ranging and dependent upon the population studied, mortality has been estimated to be as high as 54% when shock is present.1 Early administration of fluids and antibiotics are important time-sensitive treatment measures for sepsis patients.2,3 If sepsis is detected in the prehospital phase, then these treatment measures could be instituted even earlier, which may improve the patients’ prognosis. However, there is no simple diagnostic test, and screening for sepsis in the field can be challenging as laboratory data such as serum lactate or procalcitonin are not readily available.
There is a lack of research on triage tools that can predict and stratify the risk of patients suspected of having sepsis in the prehospital setting. The qSOFA tool has been found to have good prognostic value in critical care literature, but when tested in the Emergency Department (ED) triage, it had poor sensitivity in predicting sepsis-related adverse outcomes.4,5 On the other hand, the National Early Warning Score (NEWS) was found to be more accurate in predicting severe sepsis or septic shock with a sensitivity of 92.6% and a specificity of 77%, but its use is limited due to its complexity in the prehospital setting.6 Lactate is a common marker for sepsis, but it’s not always available as a point-of-care test in the field.7 In contrast, the shock index (SI), which is the ratio of heart rate (HR) to systolic blood pressure (SBP), is a simple measure that has been studied in multiple patient populations and can reflect early circulatory failure.8–10
First described in 1967, the SI provides an approximation of hemodynamic status in addition to traditional vital signs. Values approaching 1.0 are indicative of worsening hemodynamic status and shock.11 The modified shock index (MSI) has emerged as an early non-invasive measure12 that is calculated by HR divided by MAP, accounting for the diastolic function of the heart in addition to systolic function. SI and MSI are easily calculable in the field.
The aim of this research was to evaluate the usefulness of suspecting sepsis and measuring vital signs, including SI and MSI calculations, in predicting sepsis and related outcomes, such as hyperlactatemia ≥2 mmol, which is a sign of severe sepsis and a predictor of poor prognosis.13 Additionally, the study aimed to determine if these measures could predict ICU admission and 28-day mortality when applied in a prehospital setting. Our objective was to compare the ability of our prehospital sepsis protocol to predict the primary outcome of hyperlactatemia (serum lactate ≥ 2.0 mmol/L) as a surrogate for disease severity, hospital admission for sepsis, death from sepsis.
Methods
Study Design
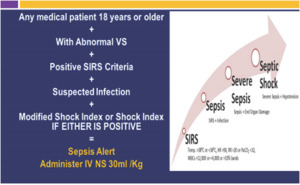
This was a prospective observational study that was conducted as part of the quality and research program of our county’s EMS system. This study was cleared by the Institutional Review Board at the University of Central Florida (#SBE-1713224). Our prehospital research registry consists of a comprehensive database and record-keeping system to collect relevant data for potential sepsis cases. Patients who met SIRS criteria with abnormal vital signs and either had suspected infection or met the shock index or modified shock index criteria, or had high-risk factors, such as being from a nursing home or having HIV, were identified as sepsis alerts. The shock index is calculated as heart rate [HR]/systolic blood pressure [SBP] >1.0); the modified shock index [MSI] is calculated as HR/mean arterial pressure <0.7 or > 1.3 (figure 1).
Study Setting and Population
As one of the largest EMS systems in our state, Polk County Fire Rescue responds to more than 115,000 calls per year, and covering a geographic footprint of over 2010 square miles. All patients aged 18 years and older who met the criteria for field sepsis alert were included in the cohort.
Measures
Our prehospital sepsis registry incorporated the following variables collected at the scene: age, gender, and vital signs. These were collected in real time. Data on serum lactate in the hospital, hospital admission, hospital diagnosis of sepsis and occurrence of in-hospital death were collected by our dedicated research officer within 30 days of the event via data capture at our mandatory quality meetings with each of the five receiving facilities.
Data analysis
Statistical analyses were performed using JMP Pro 16.0 for the Mac. Contingency analyses with Fisher’s exact test and Pearson correlation were performed on serum lactate vs. sepsis diagnosis and in-hospital death, and relative risks were calculated.
Results
Over a 24-month period, a total of 1426 patients were transported to five main receiving hospitals, with a median age of 71 years (IQR 60-80 years). The cohort was comprised of 45% female, 85% Caucasian, 14% Black, and 1% Hispanic patients. The initial shock index (SI1) ranged from 0.260 to 2.840, with a median of 1.11 (IQR 0.94 to 1.34), and 68% of patients had a positive SI1 (>1.0). The initial modified shock index ranged from 0.336 to 3.727, with a median of 1.465 (IQR 1.26 to 1.72), and 74% of the cohort had a positive MSI (<0.7, or >1.3). Among them, 3% had MSI <0.7, while 71% had MSI > 1.3. Repeat vitals during transport were available for 1321 patients (92%), and 41% had an elevated second SI (SI2). All patients with elevated serum lactate were admitted to the hospital for sepsis, and an elevated serum lactate was significantly associated with a diagnosis of sepsis (Pearson correlation, P<0.0001, relative risk of 38, 95% CI 20-72). Patients with an elevated SI were also significantly more likely to be admitted for sepsis (P<0.0001, 95% CI 0.1038 to 0.2714).
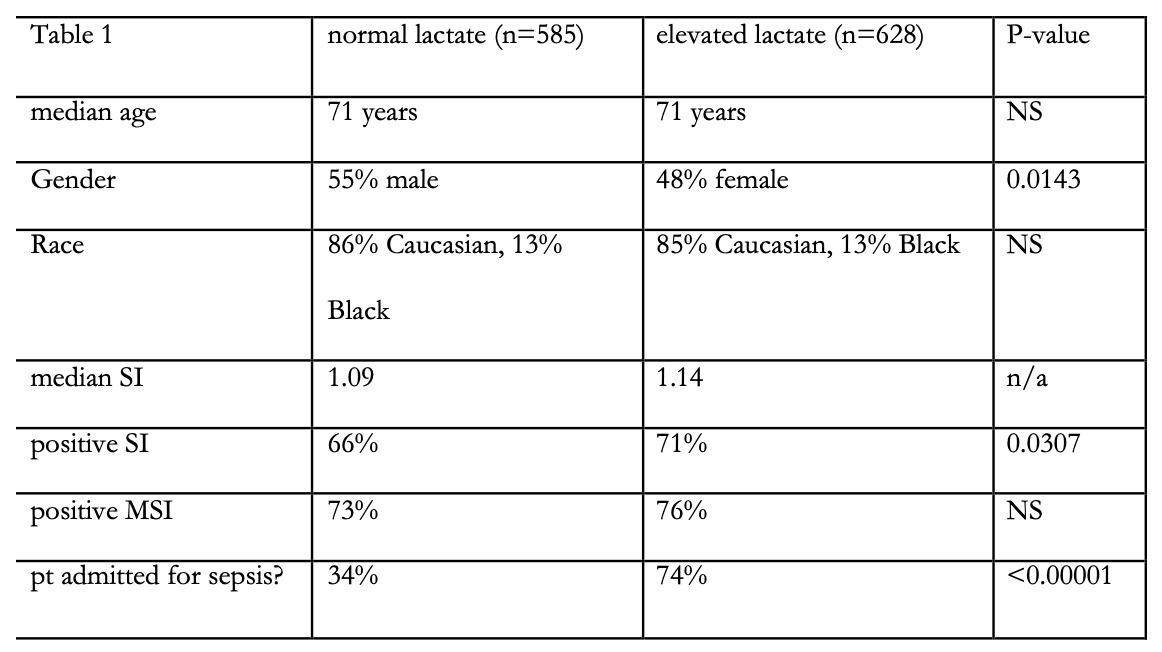
The median hospital length of stay (HLOS) was 6 days, with an IQR of 3-9 days. An increase from SI1 to SI2 was significantly associated with a longer HLOS (P<0.0001). Ultimate discharge diagnosis date was available for 1079 patients. 12.2% died during their hospital stay, while 40% had a routine discharge home. Patients with an elevated serum lactate were significantly more likely to die during their hospital stay (Pearson correlation, P<0.0001, 95% CI 0.1503 to 0.3210) with an Odds Ratio of 2.38 (95% CI 1.59 to 3.56). Table 1 summarizes the cohort by who did and who did not have an elevated lactate.
Discussion
We present the real world experience of one county’s EMS system’s outcomes using a streamlined prehospital sepsis protocol. We demonstrate that an abnormal SI which is easily calculable in the field appears to be a useful surrogate marker for sepsis, as it mirrors an elevation in ED lactate.
Other studies lend support to our work. As far back as 25 years ago, a study of ED patients found that a SI >0.9 correlated with patients triaged to a priority requiring immediate treatment, required admission to the hospital and continued therapy in an ICU9. A retrospective cohort of 3929 patients found that SI >0.875 was a reliable screening tool for the identification of hypotensive patients with sepsis who would ultimately be diagnosed with septic shock. A sensitivity of 81% and a specificity of 72% was noted for the identification of patients in whom fluid resuscitation would fail.14 In a cohort study of ED patients screened for sepsis and planned for admission, SI of≥1 was associated with 28-day mortality. Furthermore, patients with SI <0.7 were unlikely to have an elevated lactate7. A study of 238 postpartum women found a SI>0.9 to be significantly associated with sepsis, postpartum hemorrhage, and maternal mortality.5 A systematic review of 3 obstetric studies studying SI performed better than all individual conventional vital signs for predicting ruptured ectopic pregnancy.15 These studies, in addition to the data in the current study, support the concept of the shock index as a marker for sepsis. Given the time sensitive nature of treating sepsis, having a marker that can be obtained in the field is promising- we offer SI as our “invisible lactate.”
While the shock index (SI) has shown promise as a tool for predicting sepsis, there are also some limitations that should be considered. One limitation is that the SI is influenced by a variety of factors, including age, medications, and underlying medical conditions. For example, older adults may have a higher baseline heart rate and a lower blood pressure, which could lead to an elevated SI even in the absence of sepsis. Similarly, medications such as beta-blockers or calcium channel blockers can lower heart rate and potentially reduce the SI, leading to a false-negative result.
Another limitation is that the SI may not be specific to sepsis and could be elevated in other conditions that cause circulatory failure, such as hemorrhage or trauma. This could lead to false-positive results and potentially unnecessary interventions.
Additionally, the optimal cutoff value for the SI in predicting sepsis is not well-established, and different studies have used different thresholds. This lack of standardization makes it difficult to compare results across studies and may limit the generalizability of findings.
Finally, while the SI is a simple and easily calculable measure, it may not be practical for use in all clinical settings. For example, in the prehospital setting, accurate measurement of blood pressure may be challenging, and other factors such as patient movement or environmental noise could affect heart rate measurements.
Overall, while the SI has potential as a tool for predicting sepsis, its limitations should be carefully considered when using it in clinical practice. Clinicians should be aware of the factors that can influence the SI and use it in conjunction with other clinical data to guide patient care.
Limitations
Our study has notable strengths, including being conducted entirely in the prehospital setting within a county EMS system and having a robust cohort size. However, there are also significant limitations that must be considered. For instance, there is currently no established definition for an abnormal SI, as the SI has a range of values, and abnormal values varied from greater than 0.7 to greater than 1.0 in the studies reviewed. Additionally, the measurements taken in the field could have variability depending on the equipment used, and it is unclear how stable the SI and MSI are over short periods. Moreover, medications may have an impact on pulse and blood pressure, potentially altering the connection between sepsis and cardiovascular responses. Further complicating matters is the fact that geriatric patients often have complex comorbidities that may influence this relationship. Finally, while some studies adjusted the SI and MSI based on age or temperature, it remains unclear whether these adjustments are useful, particularly in patients with sepsis.
Conclusion
The shock index, which can be easily calculated in the field using standard vital signs can be a useful surrogate marker for early sepsis recognition and appears to correlate to serum lactate values. Incorporating SI/MSI into a prehospital protocol can help to expedite care and possibly improve outcomes via earlier institution of time sensitive therapy for sepsis.
Abbreviations
EMS- emergency medical services
SI- shock index
MSI- modified shock index
qSOFA - Quick Sepsis Related Organ Failure Assessment
NEWS- National Early Warning Score
HR- heart rate
MAP- mean arterial pressure