INTRODUCTION
Severe ocular surface disease and corneal ulcer can occur in a wide range of conditions such as inflammation, trauma, infection, and autoimmune disorders. This could be worsened by clinical conditions of the patient and the quality of the tear balance.1
Eye drops and tear biosubstitutes have been used as a treatment for these conditions. Amniotic membrane, an important part of the placenta, provides good structural support. It is composed of an epithelium, basal membrane, and a productive stroma. Amniotic membrane also promotes corneal healing and reduction of neovascularization inflammation. It also has anti-scarring and hemocompatibility properties. These features are attributed to growth factors, cytokines, and other molecules.2–4
The amniotic membrane can be modified and used as an extract of eye drops (AMEED).5 This modification imparts the advantage of continually providing growth factors and cytokines to heal a corneal ulcer.5,6
CASE REPORT
Ethical considerations: The patient provided written and signed informed consent for publication of this case report.
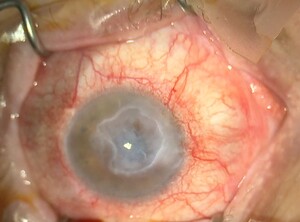
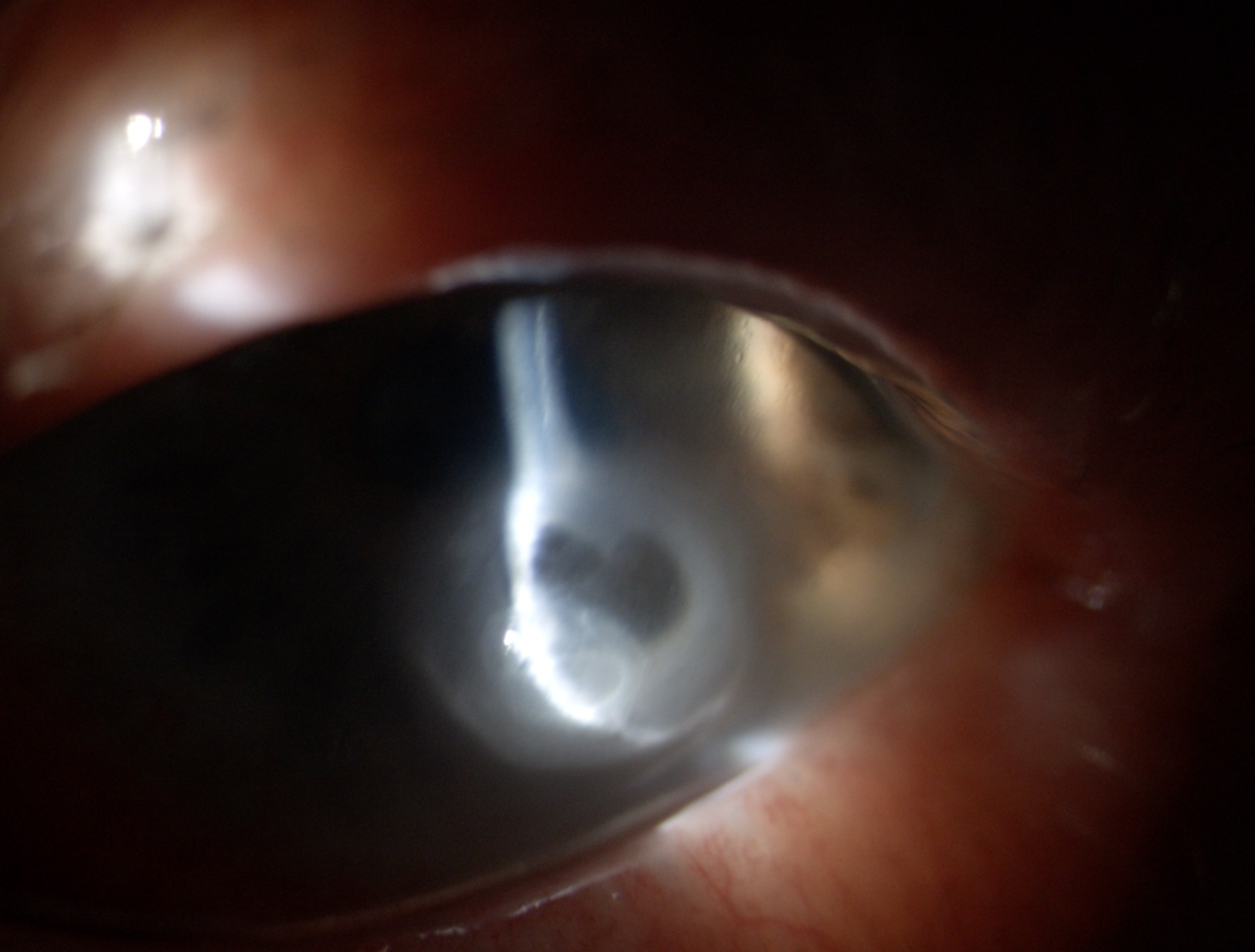
A 100 year old man came to Terrassa Hospital located in Barcelona. His past medical history was significant for diabetes mellitus, for which he was on metformin, and arterial hypertension, for which he was not on any medication. He presented with eye redness, ocular pain and foreign body sensation in his right eye [figure 1]. Because of his age, our patient did not complain about this. His son brought him to the emergency department. The main clinical findings were conjunctival redness, corneal stromal thinning [figure 2], positive Seidel sign, and ophthalmia because of a neurotrophic ulcer inadequately managed in another hospital. He had a nuclear cataract and a normal posterior pole in both eyes.
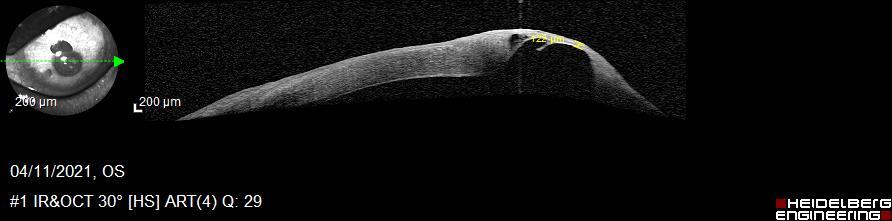
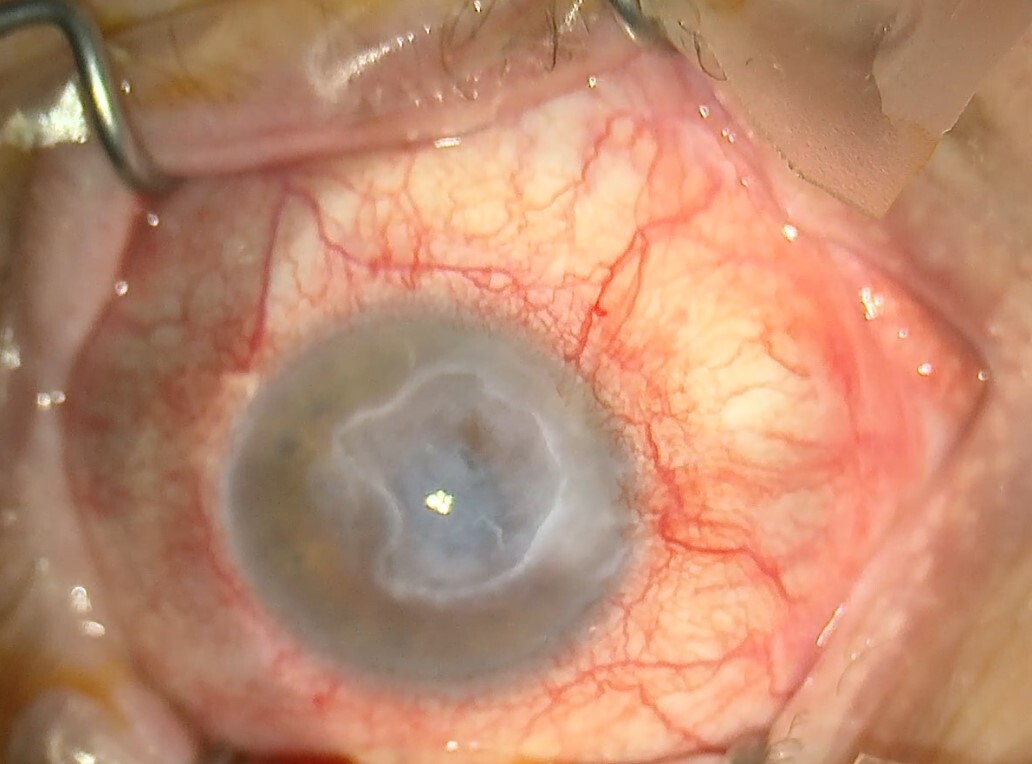
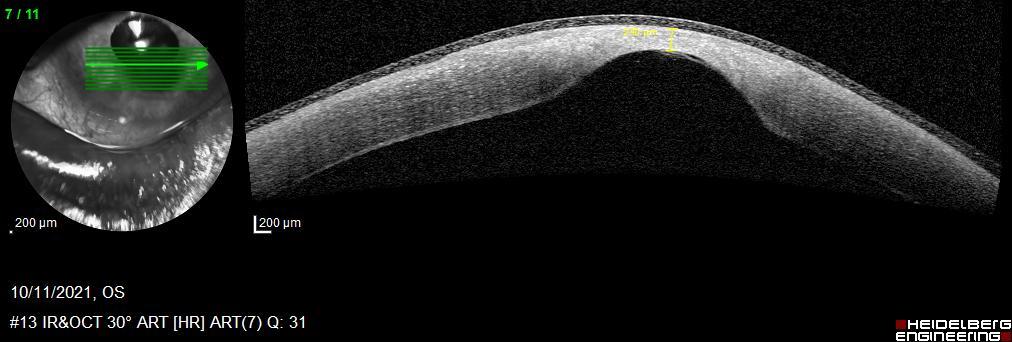
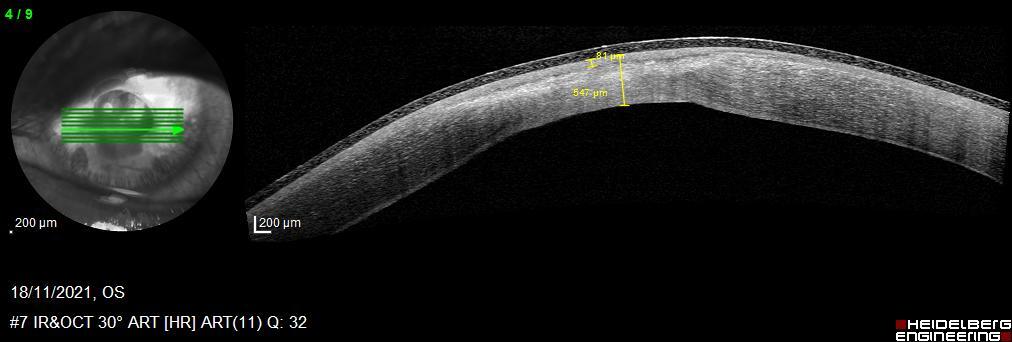
Initially, we filled the anterior chamber of the right eye with some air and patched the corneal defect with fibrin glue sealant (Tissucol ®). Then, we put a contact lens and added some topical antibiotics, and cycloplegic and artificial eye drops. Two days later, in the left eye, the corneal tissue was thinner and on the verge of perforation [figure 3]. Due to the urgency, surgical intervention was performed with an amniotic membrane graft. We used caruncular anesthesia. Two days later, there was no amniotic membrane graft. Rather, stromal thinning and descemetocele were found. We started to introduce amniotic membrane eye drops four times a day to our treatment for two months. We were not hopeful that this would work and the possibility of performing an evisceration was even raised. We followed up the evolution of the corneal thickness development with anterior segment optical coherence tomography [figure 4]. In two months the thickness went from 122 μm to 550 μm [figure 5].
Clinical background of this patient was arterial hypertension with no oral medication just diet; diabetes mellitus II with metformin as a treatment.
Discussion
Ocular surface pathology can be treated with a variety of treatments, including eye drops, antibiotics, ointments, and tear substitutes. Amniotic membrane provides an excellent treatment for epithelial defects, corneal ulcers, neovascularization, opacities, and tear film balance.7,8
Amniotic Membrane is the most internal part of the placenta. It is immersed in amniotic liquid; both have plenty of healing properties. The majority of these features belong to its biomolecules: Collagen types (I, II, IV, and V) and Growth factors such as epithelial growth factor (EGF), transforming growth factor (TGF), and hepatocyte growth factor are involved in corneal healing. Together, they contribute to restoring the corneal surface. Amniotic membrane also downregulates proinflammatory cytokines.9,10
Amniotic Membrane has been used in different specialties since 1910 for skin transplantations, wound care, urology, orthopedics, and dentistry.11–13 It was only around 1990 that its use in ophthalmology started arising.13,14 It can be used fresh for an amniotic membrane graft or transplant or could be extracted and used for eye drops. The use of amniotic membrane eye drops, specifically formulated for ophthalmic applications, presents an exciting avenue for non-invasive treatment of conditions such as dry eye disease and persistent corneal defects. The anti-inflammatory and regenerative properties of amniotic membrane eye drops make it a valuable addition to the armamentarium of ocular therapeutics, as seen in our patient.
While further clinical trials are needed to validate the full scope of applications and efficacy of amniotic membrane eye drops, the existing evidence suggests their potential as adjunctive treatments for various ocular surface disorders. Additionally, the ongoing research and development of commercial amniotic membrane derivatives offer promising prospects for expanding treatment options in ophthalmic care.8–13
Conclusion
The therapeutic potential of amniotic membrane extract and eye drops in ophthalmology holds promise for enhancing corneal healing, managing ocular surface diseases, and potentially improving patient outcomes. Continued research and clinical validation will further elucidate the specific applications and benefits of these innovative treatment modalities in the field of ophthalmic care.