RESEARCH ABSTRACT WINNERS
1st Place Faculty/Fellow:
Kimberly Alford, MD and Allison Schiller, DO
Development and Implementation of an Advanced Teaching Elective for Emergency Medicine Residents
1st Place Resident:
Darielys Mejias, MD
Trivia Night: Disaster Medicine Edition
1st Place Student:
Meghana Konda
Epidemiology of Musculoskeletal Injuries in Archers
2nd Place Student:
Ethan Nichols
Predictors of TBI Severity from Motor Vehicle Collisions
3rd Place Student:
Jasra Elahi
Upper Extremity Injuries Due to Martial Arts
RESEARCH ABSTRACTS
1 Development and Implementation of an Advanced Teaching Elective for Emergency Medicine Residents
Kimberly Alford, MD, Allison Schiller, DO, Donald Norris, MD
East Carolina University Brody School of Medicine
Objective
Emergency medicine residents interested in medical education often have limited training in teaching skills including curriculum development, presentation design and delivery, bedside teaching, and delivery of feedback. A pivotal 2006 paper in Academic Emergency Medicine presented a curriculum for residents as teachers in emergency medicine. Additional papers have focused on initiating a curriculum for foundational teaching skills. At our institution, a required teaching rotation emphasizes these skills. However, we wanted to create an advanced teaching elective for senior residents interested in academic medicine.
Methods
After assessing the resident’s goals, we developed an individualized plan identifying four areas within our clerkship where various teaching modalities could be applied: developing and presenting core content lectures, creating a procedural guide, leading simulation-based learning, and bedside teaching. The resident was observed and evaluated by the clerkship director, associate program director and education division chief. A debriefing session was held with the resident and evaluators to obtain and deliver feedback.
Results
In contrast to the required teaching rotation, the elective concentrated on the resident’s educational goals as well as the academic needs of the clerkship. Resident goals included leading simulation activities and advancing bedside teaching. The clerkship needs to be focused on content which included creating and delivering three lectures, the development of a question bank for existing student modules, and the creation of an airway skills guide. All objectives, including evaluation and debriefing, were successfully completed during a 4-week rotation.
Conclusions
The ACGME core competencies include the role of physician as educator. Many programs incorporate a curriculum for EM residents to practice foundational teaching skills. We sought to further develop these skills in a safe environment for residents with academic career goals. As we continue to develop this elective, we plan to expand instruction on adult learning theory, cognitive errors, and delivering feedback to learners.
2 Trivia Night: Disaster Medicine Edition
Darielys Mejias-Morales, MD; Shayne Gue, MD; Andrew Little, DO, David Lebowitz, MD, Latha Ganti, MD
UCF/HCA Florida Osceola Hospital Emergency Medicine Residency, Kissimmee, FL
Introduction/Background
Gamification has been shown to improve learning by promoting motivation, engagement, and increased knowledge retention. Mass casualty incident (MCI), disaster preparedness, and event medicine are sometimes overlooked topics for the Emergency Medicine in-training exam (ITE). This trivia quiz competition incorporates gamification into residents’ educational didactics curriculum in preparation for board exams.
Educational objectives
Review ITE content using a jeopardy-style trivia competition. Our goal is to promote collaboration and gain consensus among emergency medicine residents to answer board-style questions, while also preparing them to face real-life patient encounters.
Curricular design
Jeopardy-style trivia game designed using playfactile.com as a quiz competition among residents. 55 residents were divided into six teams, each team with an equivalent number of interns, juniors, and seniors. The game included a combination of short questions and board-style case scenarios for fast recall and reinforcement of residents’ knowledge about MCI/disaster/event medicine. This “Disaster Trivia” was incorporated into our weekly didactics. The duration of the session was 75 minutes. This educational method was chosen to promote engagement and teamwork in an approach to both, fast recall of material and structured answering of board-style questions. This curricular design also provides the opportunity for instant knowledge feedback and reinforcement via short discussions after each trivia question.
Impact/Effectiveness
Post-activity survey evaluation was accessed using a QR code. Residents reported that, compared to other educational methods, “Disaster Trivia” was more engaging, better motivated them to learn, and better challenged them to learn these ITE topics. 88% of residents also reported feeling better prepared to manage a real-life MCI/disaster/event medicine scenario as a result of their participation in this activity.
3 Epidemiology of Musculoskeletal Injuries in Archers
Meghana Konda
Lake Buena Vista High School, Orlando, FL
Objective
While it is considered a generally safe sport, archery can lead to injuries that contribute significantly to the desensitization of the upper extremities in an individual. Unfortunately, tendinitis, sprains, and lacerations are still extremely common even with proper precautions. Archers have a 4.4% average chance of being injured during their training periods. By studying mechanisms of injury and correspondence to age, the goal of the study is to encourage innovative design for equipment manufacturers and educate caregivers, health care workers, on risk mitigation and prevention.
Methods and Materials
The National Electronic Injury Surveillance System Database was queried to analyze archery-related upper extremity injuries that occurred in all ages with 10 year age groups between 2013 and 2022.
Results
Approximately 43,083 injuries occurred over a 10-year span. While 8,038 women were injured, men were injured 4.4 times more frequently with 35,367 men being injured annually. Injured sites in men included the finger (66%), hand (17%), face (6%), shoulder (5.4%), and foot (5.1%). All injuries in women were finger related injuries. The top diagnoses included lacerations (58%) in men and (100%) in women. Other top diagnoses in men included fractures (13%), contusions and abrasions (7.5%), foreign body (5.9%), puncture (4.9%), and strains/sprains (4.9%).
Conclusion
The study identifies that lacerations were the most frequently diagnosed archery related injuries. Additionally, the fingers were the most common site of injury in both genders. These results provide new information about the types of safety gear that should be implemented and manufactured to prevent further injuries, and this data helps anticipate injury profiles seen in emergency settings. Future research should study why lacerations are strongly associated with archery related injuries, so safety features can be optimized and gear designs can appropriately be altered.
4 Predictors of TBI Severity from Motor Vehicle Collisions
Ethan Nichols
Windermere Preparatory High School, Windermere, FL
Objective: Motor vehicle collisions are the second most common cause of traumatic brain injury (TBI). In this study, the authors sought to determine the predictors of TBI severity in adult patients involved in motor vehicle collisions (MVC).
Methods: This is a retrospective observational cohort of adult patients (≥18 years) who sustained a TBI due to an MVC. Demographic, pre-hospital, and clinical data were collected. Statistical analyses were performed using JMP 16.0.
Results: The cohort consisted of 816 patients. 473 (58%) were male, with a median age of 31 (IQR = 23-49), while female patients had a median age of 33 (IQR = 22-48). Of these patients, 153 (19%) had moderate or severe TBI (GCS<12), and 663 (81%) had mild TBI (GCS≥12). A multivariate model was built using the variables age, sex, alcohol consumption before the injury, loss of consciousness (LOC), associated seizure, associated vomiting, alteration in consciousness (AOC), and post traumatic amnesia (PTA). This was a robust model in which an R2 of 40.37% was obtained.
The following factors were significantly associated with TBI severity: male sex (P = 0.0215, CI = 1.088-3.166), alcohol consumption prior to injury (P < 0.0001, CI = 1.754-4.912), loss of consciousness (P = 0.0562, CI = 0.9771-5.985), use of seatbelt (P = 0.0007, CI = 0.2177-0.6679), alteration of consciousness (P < 0.0001, CI = 7.621-63.625), and post-traumatic amnesia (P < 0.0001, CI = 2.212-10.208).
Conclusion: Peri-injury features such as post-traumatic amnesia, alteration of consciousness, and behaviors such as wearing a seatbelt and not drinking alcohol prior to driving appear to be significant predictors of having more severe head injury. These data support a call for action to implement more widespread injury prevention, seatbelt use education and advocacy, and prevention of alcohol prior to entering a motor vehicle.
5 Upper Extremity Injuries Due to Martial Arts
Jasra Elahi
Lake Buena Vista High School, Orlando, FL
Given the rise of Martial Arts within the fitness and recreational industry, it is important to study trends in injury and to note that practicing martial arts comes with a risk of injury, particularly to the upper extremities. By studying consumer product-related injuries to the upper extremities and addressing the current gap in the literature, future martial arts equipment can come with increased safety features, better provide information to healthcare providers treating such injuries, and improve risk mitigation through the Consumer Product Safety Commission. The National Electronic Injury Surveillance System Database was analyzed to collect data on martial arts equipment-related injuries on the upper extremities within the last 10 years. Over the most recent span of 10 years (2013-2022), there were approximately 78,680 injuries reported to the ED. The majority of them took place in the year 2013 (12.8%). Men were 2.4 times more likely to get injured than women. Injuries peaked in the age group 10-19-year-olds (33%) and particularly in the age 12 (4.8%). The upper extremity most commonly affected was the shoulder (29.1%), and the most common diagnosis group was a fracture (29.2%). Most injuries presented to the emergency department were not hospitalized (98.7%). This study highlights the occurrence of upper extremity injuries due to martial arts within the last 10 years and provides new information on the prevalence of such injuries. The results better explain that these injuries are usually non-severe and most commonly affect adolescent males; however, future research should explore performance-based recovery post-injury and long-term pain.
6 Access to Healthcare in Rural Communities: A Bibliometric Analysis
Ariya Natarajan
Memorial High School, Eau Claire, WI
Introduction: Access to healthcare is defined by being able to receive regular checkups, specialist appointments, immunizations, procedures, and surgeries within a reasonable timeframe and without restrictive barriers.
Methods: The Web of Science database was used to collect 4,745 articles published relating to the keywords “rural”, “access”, and “healthcare”. These articles then underwent bibliometric cataloging by country, journal, and keyword using VOSviewer 1.6.19.
Results: Between the years 2015 and 2022, the United States emerged as the predominant publisher in the field. From 2015 to 2019, the United States accounted for 47 percent of the total articles published. However, in the subsequent years of 2020 to 2022, there was a slight decline of 3 percent in the volume of U.S. publications. Australia secured the second position in terms of publications within the aforementioned timeframe of 2015 to 2022. England had the third most publications during the time between 2015 to 2022. The prevalence of articles containing the keyword “disparity” ranged between 7 percent and 12 percent throughout this period. Plus One exhibited prominence by contributing 5.025381 percent of all publications pertaining to access to rural medicine during the years 2015 to 2019 thereby establishing itself as the leading publisher in this domain. However, in 2020, the International Journal of Environment suppressed Plus One by publishing the highest number of articles related to rural healthcare. Subsequently, the BMC Health Services Research claimed the leading position in the years 2021 to 2022.
Conclusion: An exploration of who is contributing to the discussion of access to healthcare in rural communities shows that the field and number of publications is growing, and that a focus on disparities is emerging, creating an environment surrounding rural health focused on researching equitable care.
7 The Effect of Anticoagulants and Antiplatelets on the Severity of Traumatic Brain Injuries
Jai Gupta
Seminole High School, Sanford, FL
Background
Anticoagulants and antiplatelets are widely prescribed for a variety of conditions to prevent thromboembolism. Unfortunately in the setting of head injury, they can result in intracranial hemorrhage.
Objective
This study aims to analyze the burden of anticoagulants and antiplatelets on the outcomes of traumatic brain injury.
Methods
This was a retrospective cohort analysis of consecutive adult patients who presented to the emergency department for a TBI. TBIs were categorized as mild, moderate, and severe based on the Glasgow Coma Scale. Statistical analysis was performed in JMP 16.0
Results
The median age of the cohort of 3,021 adults was 39 years (IQR 24-59). 872 (28.8%) were >55 years of age, the age qualifier for trauma alert in our state. 59.8% of the cohort were men (1808) and 339 adults (11.2%) were on anti-platelets or anticoagulants. 1439 (47.6%) suffered a TBI from a fall while 1084 (35.9%) had a TBI secondary to a motor vehicle collision. A total of 958 (31.7%) people suffered an intracranial bleed. 11.8% of the TBIs were severe, 3.2% were moderate, and 85% were mild. In a multivariate model controlling for age, sex, mechanism of injury, and TBI severity, there is a significant association between patients taking anti-platelets and anti-coagulants and an increased likelihood of intracranial hemorrhages (P = 0.0356, 95% CI -1.73 to -0.16).
Conclusion
The use of anti-platelets and anti-coagulants imparts excessive morbidity in adults with TBIs across the range of injury severity.
8 Convergence Insufficiency Correlations in Mild Traumatic Brain Injury
Kavya Devani
Vista Ridge High School, Austin, TX
Introduction
Traumatic Brain Injury (TBI) is damage to the brain resulting from force to the skull and is commonly caused by sports injuries and motor vehicle accidents. This study focuses on the convergence insufficiency score (CSI) which measures the ability of the eye to maintain focus on an object using binocular cues. CSI could cause patients to only be able to see from one eye or experience double vision. TBI is a common cause of CSI but oculomotor function is rarely tested in the Emergency Department (ED). The purpose of this study was to see the relation of CSI as a predictor of prognosis and as an outcome of the TBI itself.
Methods
This study was a secondary analysis of a prospective observational data set of mild TBI (Glasgow coma scale score 13-15) that presented to the ED. Data analysis was done using JMP 16.0.
Results
The cohort consisted of 58 men and 58 women. Females showed a higher median CSI score of 14 while males had a median CSI score of 10. In a multivariate model the strongest predictors of CSI were post-head injury headaches (p<0.0001, 95% CI 4.47-11.90), post-traumatic amnesia (p= .0011 95% CI 3.40 - 13.10), different thinking (p = .0053, 95% CI 2.89-16.1), and disorientation (p-value = .0059, 95% CI -19.92 to -3.45) with a total r squared value of 36.2%. In univariate models CSI was shown to be a predictor for the likelihood of being admit (p= .0378, 95% CI .002-.078, r2=3.1%), new symptoms at 30 days follow-up (p = .0322, 95% CI .001-.0303, r2=7.9%)
Conclusion
This study suggests CSI has a correlation to symptomatic prognosis and can be used as a quick and easy tool to risk stratify ED patients who present with mild TBI.
9 Difference Between Sex in Signs of Return of Spontaneous Circulation (ROSC) after Out Of Hospital Cardiac Arrest
Arya Ali
Marietta, Georgia
Background
Cardiac arrest is an unfortunate event with poor prognosis. There is some suggestion that women may fare better than men. This study of out of hospital cardiac arrest sought to determine if a difference indeed exists.
Methods
These prospective data are from our Emergency Medical Staff (EMS) agency’s Cardiac Arrest Registry Enhance Survival (CARES) registry. Information on Cardiopulmonary Resuscitation (CPR) metrics, sex, and outcomes including return of spontaneous circulation (ROSC) were recorded. All peri-arrest rhythms including ventricular fibrillation, PEA, and asystole were included.
Results
A total of 1,364 patients were in the dataset. 532 (39%) were women. The median age for women was 67.5 years (IQR 53.25-77) and 65 years for men (IQR 52-76 years). The frequency of ROSC amongst women was 17.9% whereas for men it was 14.4%. A multivariate model including whether arrest was witnessed, the first monitored rhythm, sex, age, time to first CPR, whether epinephrine and hypothermia care was given and whether defibrillation occurred, demonstrated women had significantly higher ROSC (p=0.0021, 95% CI 0.0947 to 0.4293).The odds ratio for women having ROSC compared to men was 1.64, suggesting they are 62% more likely to have ROSC.
Conclusions
The odds ratio for women having ROSC compared to men was 1.64, suggesting they are 62% more likely to have ROSC, even after controlling for other factors known to improve ROSC rates prompt CPR and hypothermia care.
10 Burden on Cancer Caregivers
Avi Gupta
Seminole High School, Sanford, FL
Background/Objective
Cancer is a debilitating disease for which patients often need caretakers to help them live their lives and complete basic activities. This study aims to characterize the burden of the caretaker.
Methods
A 14 question survey of was sent out to randomly selected United States cancer caretakers to analyze the social, emotional, and physical burden of their caretaking.
Results
The results show that a majority of caretakers are direct family to the patient (69.5%). The patients’ cancers are often in early stages with about 54.5% having stage 1 cancer and 22.5% having stage 2 cancer while only 8.5% had stage 3 cancer and 17.8% had stage 4 cancer. When asked about their motivation, caretakers most often do it because of love (58.82%) with family responsibilities/duty being the second highest reason (35.56%). When asked about their biggest burden, many caretakers said that grief was the biggest issue (30.50%) with mental health issues also being troublesome (28%). 75.6% of respondents said that being a cancer caretaker has negatively impacted their mental health from either anxiety (37.29%), depression (33.9%), or other conditions (4.41%). When asked about negative impacts of being a caregiver, 43.5% stated they faced high financial costs to give care, 35% stated they faced a lack of social support or lost friends, while 33% stated they had negative physical impacts. The amount of participants who face overwhelming or high stress nearly quintupled from baseline, from 13% to 59.5%.
Conclusion
This cross-sectional survey of US adults demonstrates that there are clear negative impacts on cancer caregivers to their physical, financial, social, and mental health. These data underscore the importance of taking care of patients’ caregivers.
11 Racial Disparities in Subjective Cognitive Decline and its Implications among Alzheimer’s Caretakers
Dylan Wang
Trinity Preparatory School, Winter Park, FL
Background/Objective: Alzheimer’s disease is a prominent neurodegenerative disorder characterized by cognitive decline and memory loss. Variations in subjective cognitive decline among Alzheimer’s patients, often reported by caregiver, may stem from cultural, socioeconomic, healthcare access, and genetic factors. This study investigates racial disparities in subjective cognitive decline reported by caregivers and their implications.
Methods: In this study, data from 12,627 Alzheimer’s caretakers from the CDC’s Alzheimer’s Disease and Healthy Aging Data Portal were analyzed using JMP software. Caregivers reported patients’ cognitive decline for various racial categories: Asian/Pacific Islander, Black, Hispanic, Native American/Native Alaskan, and White. Fit model tests and distribution analyses were employed to assess disparities in symptom severity. The study focused on four key questions regarding symptom prevalence and healthcare communication to assess the degree of symptoms the patients were experiencing.
Results: Significant disparities in symptom severity reported by Alzheimer’s caretakers were observed among the racial groups analyzed. The symptom severity ranked from least to most severe is the following: White, Asian/Pacific Islander, Black, Native American/Native Alaskan, and Hispanic patients. There was variance when it came to communication with healthcare providers, as the Asian population had the lowest communication rates. These findings underscore the need for targeted interventions considering cultural differences. It is important that tailoring healthcare approaches for different racial backgrounds is happening as a remedy to this gap in communication.
Conclusion: Due to cultural, socioeconomic, genetic factors, and others, there were significant observed disparities. Tailoring interventions to these diverse populations is crucial to address these inequities.
12 The Impact Of Post-Traumatic Stress Disorder(PTSD) on Caretakers in the United States
Ananya Surabhi
John Foster Dulles High School, Sugarland, TX
First diagnosed in 1980 by the American Psychiatric Association (APA), post-traumatic stress disorder (PTSD) is a serious mental health concern that can occur after patients have experienced or witnessed a traumatic event. Caregivers play crucial roles in the recovery journeys of those facing mental instabilities. They provide emotional, social, and physical support to patients with PTSD.
The authors created a survey of twelve questions and collected data from 200 caretakers regarding how taking care of PTSD patients impacts their social, mental, and physical health. Other statistics that were collected included key demographic and background information.
The results indicate that most PTSD caregivers are family members (48.5%). PTSD often strains the caretaker’s relationship with the patient (44%), and 45.5% of caregivers reported sleeplessness. 41% reported that they were diagnosed with depression after becoming a caretaker for a patient with PTSD. 37% reported that they had less emotional stability since becoming a caregiver. 35.5% of caretakers also reported that they had financial stress because of becoming a caretaker. Most caretakers cooked and cleaned for their patient (73%) and took them to a doctor/therapist (66%). The primary motivator for caregivers was love (81.5%). Stressors for the caretaker include worry for the patient (65%), financial worries (45.5%), and their own health (29.5%). To cope with stress, caretakers reported that they did physical activity (25.5%) and went to therapy (25%). 22% reported that they consumed entertainment to relieve their stress.
While many caregivers have coping methods to alleviate the burden of caring for a patient with PTSD, the clear negative impact PTSD has on caretakers affects their mental and physical health. Because there is no cure for PTSD, caregivers require additional support to continue caring for their patients and maintaining a stable life.
13 The Epidemiology of Adolescent Volleyball-Related Injuries
Aaditya Jandhyala
Orlando Science High School, Orlando, FL
Objectives: Playing sports is crucial to adolescents as a source of entertainment, a factor in improving mental health, and a way to promote physical development. However, sports, including volleyball, have an inherent risk of causing injuries to its players. The objective is to determine the most common locations, types, and outcomes of volleyball injuries in adolescent athletes so that more people are aware of how these injuries occur. This would encourage volleyball athletes to be more mindful of these injuries when playing.
Methods: The National Electronic Injury Surveillance System (NEISS) was used to analyze injuries in adolescents (ages 10-19) that occurred due to volleyball between the years 2013 and 2022.
Results: Approximately 347,395 volleyball injuries occurred in adolescents between 2013 and 2022, with the median age of patients being 15 years old. 274,003 patients were female (78.9%) while 73,392 patients were male (21.1%). 59,530 had injuries in the head or neck (17.1%), 141,660 in the lower extremities (40.8%), and 119,230 in the upper extremities (34.3%). 151,364 patients had sprains or strains (43.6%), 35,760 had fractures (10.3%), 36,804 had contusions or abrasions (10.6%), and the rest of the patients had other injuries. 342,567 patients were treated and released (98.6%), 2049 patients were left without being seen (0.6%), and 1648 patients were hospitalized (0.5%).
Conclusions: This study shows that volleyball players are most vulnerable to getting sprains, strains, fractures, or bruises in the upper or lower extremities. While there are more injuries in adolescent females, this is likely because a majority of volleyball players between the ages of 10 and 19 are female. Further study may be done to identify how volleyball causes these injuries in an effort to prevent them.
14 Epinephrine and Hypothermia in the Field Are the Cornerstones of Achieving ROSC after PEA Arrest
Anitej Akella
Orlando Science High School, Orlando, FL
Objective
Pulseless electrical activity (PEA) has a national survival-to-discharge rate of 2-5%, indicating a poor prognosis. This study examines which factors most significantly affect the return of spontaneous circulation (ROSC) and sustained ROSC.
Methods
This is a prospective observational study that uses the Cardiac Arrest Registry to Enhance Survival (CARES) database for our EMS agency, and comprise all PEA arrests over age 18. ROSC was defined as the return of spontaneous circulation by a palpable pulse for at least 30 seconds. Sustained ROSC means that the patient maintained a pulse through the end of the EMS response and made it to the hospital alive.
Results
In the cohort of 250, 233 (93.2%) were given epinephrine. There are 153 (61.2%) males and 97 females (38.8%), and 111 (45.1%) received hypothermia care. A logistic fit model, including sex, age, the time between arrest and arrival of emergency medical services (EMS) on the scene, whether the arrest was witnessed, whether hypothermia care was provided, the time to cardiopulmonary resuscitation (CPR), and whether epinephrine or amiodarone was used. No patients were excluded from any of the models made during this study. Female sex (P= 0.0195, 95% confidence interval (CI) of 0.060-0.678), hypothermia care in the field (P=0.0265, CI of -0.676 to -0.045), and epinephrine (P=0.0206, CI of 0.172-1.763) were the most statistically significant variables for whether or not ROSC will be achieved. Female sex (P=0.0084, CI of 0.109-0.745), hypothermia care (P=0.0492, CI of -0.651 to -0.001), and epinephrine (P=0.0181, CI of 0.163-1.740) were the most statistically significant variables for whether or not ROSC will be sustained. The R-squared value for achieving ROSC is 0.0785, and the R-squared value for achieving sustained ROSC is 0.1013. Females are approximately twice as likely to achieve ROSC as males, patients who are given epinephrine are approximately six times are likely to achieve ROSC as patients who are not given epinephrine, and patients who receive hypothermia care in the field are approximately twice as likely to achieve ROSC as those who do not.
Conclusions
In order of importance, administering epinephrine, female sex, and receiving hypothermia care are the strongest predictors of achieving and sustaining ROSC.
15 Factors Influencing Patient Satisfaction with Total Joint Replacement Surgery
Dhrupad Ponnamaneni
Moorestown Friends School, NJ
Background: Replacement arthroplasty surgery is a surgical procedure that is needed to restore the activity of a joint. Patient satisfaction regarding arthroplasty surgery is influenced by post-operative complication rate, ability to afford care, and quality of interaction. In this study, we assessed patients’ postoperative complications, mobility, and pain management as proxies for their overall satisfaction with TJR.
Methods: An anonymous web-based survey was conducted for patients who had undergone any total joint replacement surgery in the US. Respondents were adults living in the United States.
Results: 180 individuals met the inclusion criteria and responded to the survey. Age, education, gender, and race were fitted against the patient satisfaction level with the surgeon. While education [P=0.4720], gender [P=0.5097 ], and race [P=0.8183] were not significant, age in years [P=0.02340] was predictive of overall satisfaction levels [R2=0.0213]. When controlling for BMI, infection [P=0.0164], nerve damage [P=0.0250], delayed healing [P=0.0024], hematoma [P=0.0497], were more likely to occur in participants who have had a knee replacement, as compared to shoulder and hip replacement surgery. When controlling for mobility before surgery vs. mobility after surgery [P=0.0114], patients who selected the highest level of mobility before surgery were likely to select the highest level of mobility after surgery. Medicaid, Medicare, private insurance, employer-based insurance, and no insurance were fitted against the patient’s self-reported difficulty in paying for their treatment/care. Although employer-based insurance [P=0.0790] was not significant in predicting difficulty in paying for the surgery, patients with Medicaid [P=0.0280], Medicare [P=0.0200], or private insurance [P=0.0343] had greater difficulty the surgery was to pay for.
Conclusion: In this cohort, older patients were associated with having improved satisfaction with the surgeon who performed their joint replacement. Complications were higher in patients who underwent a knee arthroplasty compared to a shoulder or hip arthroplasty.
16 Prevalence of Craniofacial Injuries in Elderly Populations
Pranav Chepyala
LinnMar High School, Marion, Iowa
Introduction: Recognizing and understanding risk factors for craniofacial injury in the elderly is of paramount importance in prevention. This research aims to investigate the prevalence of craniofacial injuries in connection with extrinsic preventable factors, particularly identifying common household products that pose the greatest risk for such injuries.
Materials and Methods: This study was done via the utilization of the 2013-2022 National Electronic Injury Surveillance System (NEISS). Data gathered included patient age, injury type, cause of injury, and year of incidence. ‘Elderly’ was defined as an individual of 65 years of age or older.
Results: There was a total of 9,703,688 estimated national cases of elderly craniofacial injury from 2013 to 2022. 5,888,112 (60.68%) of these occurred in females. In descending order, the five most common items responsible for craniofacial injury in the elderly are floors/flooring Materials (3,741,706, 30.92%), beds/bedframes (1,250,396, 10.33%), stairs/steps (907,92, 7.50%), chairs (546,697, 4.52%), and tables (453,989, 3.75%). These top five account for roughly 57% of all cases. The five most common presenting diagnoses were Internal Injury (2,957,095, 40.21%), Lacerations (1,435,926, 19.53%), ABR (1,191,008, 16.20%), Fracture (568,842, 7.74%), and Hematoma (355,871, 4.84%).
Conclusions: Out of the roughly ten million cases of craniofacial injury in the last decade, approximately three-fifths have happened to women. The majority of injuries occur in a home setting. The overwhelming majority of cases were related to the product code 1807-floors or flooring materials and the largest diagnosis was internal injury by a wide margin. Evidently, there is a large population of elderly patients that suffer from craniofacial injuries related to objects and items that permeate within their living residences. The elimination of excess elderly craniofacial injury can be achieved by reducing fall risk factors in the immediate vicinity of the elderly.
17 Use of Helmets mitigates TBI severity in School-aged Children
Sidhartha Ramlatchan
Drexel University, Philadelphia, PA
Many children use recreational vehicles (such as bicycles) daily but required use of helmets in this vulnerable pediatric population is a controversial topic and laws are not universally in place. Our findings emphasize the importance of proper safety precautions during the operation of recreational vehicles. We conducted an IRB-approved observational cohort study of patients (including children aged 5-17) who came to the emergency medicine department of a healthcare facility with a Level-1 trauma center with the primary diagnosis of TBI. In the cohort, 148 patients reported the use of a recreational vehicle prior to injury (with the most common one being ATVs, followed by bicycles and motorcycles). Helmet use was assessed in 91.3% of this population. Only 17% of bicycle and 16% of ATV associated injuries reported helmet use. Seventy-seven percent of motorcycle accidents reported helmet use. Eighty-eight percent of our cohort had a mild TBI (GCS=13-15), 2% had moderate TBI (GCS=9-12), and 10% had severe TBI (GCS<;9).Of those with severe TBI, only 7% reported helmet use and 60% were due to ATV accidents. Regression analysis in our population showed helmet use to be protective of hospital admission (p=0.0004), abnormal CT findings (p=0.008), specifically calvarial fracture (p=0.023), controlling for age and gender. These data support the importance of helmet use in a pediatric population as a protective device. The majority of states do not have laws requiring helmet use on recreational vehicles, and our data help to support policies requiring use of this protective measure.
18 Predictors of Brain Computed Tomography (CT) Scan abnormalities in mild Traumatic Brain Injury (mTBI)
Sihi Vasista
Seminole High School, Sanford, FL
Objective/Introduction: Mild Traumatic Brain Injury (mTBI) is a common occurrence that results in neurological dysfunction. mTBI is defined as a Glasgow Coma Scale (GCS) of 13-15. This study aims to identify predictors associated with the presence of brain CT abnormalities in patients with mTBI.
Methods: Secondary analysis of a retrospective observational cohort presenting to the emergency department with mTBI that occurred within 24 hours prior to presentation.
Results: A total of 2786 patients met the inclusion criteria, of which 2548 (91%) had a brain CT and 698 demonstrated abnormal findings. The most frequently observed CT abnormalities were bleeding (638) and fractures (190). Multivariate logistic regression analysis revealed several significant predictors associated with the presence of brain CT abnormalities including older age [p<0.0001, 95% CI 0.0066 to 0.0081], male sex [p<0.0001, 95% CI 0.00491to 0.00548], loss of consciousness, associated vomiting, alteration of consciousness (aoc) [p= <0.0001, 95% CI 0.008 to 0.939] and post traumatic amnesia (pta) [p<0.0001, 95% CI 0.03072 to 0.09682]. This was a robust model with an R² of 14.9%.
Conclusion: In this retrospective analysis, loss of consciousness, aoc, pta, associated vomit, and associated seizures, were found to be significant predictors of having an abnormal brain CT. These findings highlight the importance of considering these factors when determining the necessity of brain CT scans in patients with mTBI. Early identification of individuals at a higher risk of CT abnormalities may assist in appropriate management and allocation of healthcare resources. These findings may also help to inform clinical decision rules.
19 Bibliometric Analysis of ChatGPT in Medicine
Sharanya Gande
Academy at the Lakes, Land O Lakes, FL
Introduction: The emergence of AI chat programs has opened two distinct paths, one enhancing interaction and another potentially replacing personal understanding. Ethical and legal concerns arise due to the rapid development of these programs. This paper investigates academic discussions on AI in medicine, analyzing the context, frequency, and reasons behind these conversations.
Methods: The study collected data from the Web of Science database for articles containing the keyword “ChatGPT” published from January to September 2023, resulting in 786 medically related journal articles. The inclusion criteria were peer-reviewed articles in English related to medicine.
Results: The United States led in publications (38.1%), followed by India (15.5%) and China (7.0%). Keywords such as “patient” (16.7%), “research” (12%), and “performance” (10.6%) were prevalent. The Cureus Journal of Medical Science (11.8%) had the most publications, followed by the Annals of Biomedical Engineering (8.3%). August 2023 had the highest number of publications (29.3%), with significant growth between February to March and April to May. Medical General Internal (21.0%) was the most common category, followed by Surgery (15.4%) and Radiology (7.9%).
Discussion: The prominence of India in ChatGPT research, despite lower research funding, indicates the platform’s popularity and highlights the importance of monitoring its use for potential medical misinformation. China’s interest in ChatGPT research suggests a focus on NLP AI applications, despite public bans on the platform. Cureus’s success in publishing ChatGPT articles can be attributed to its open-access, rapid publication model. The study identifies research trends in plastic surgery, radiology, and obstetric gynecology, emphasizing the need for ethical considerations and reliability assessments in the application of ChatGPT in medical practice.
Conclusion: ChatGPT’s presence in medical literature is growing rapidly across various specialties, but concerns related to safety, privacy, and accuracy persist. More research is needed to assess its suitability for patient care and implications for non-medical use. Skepticism and thorough review of research are essential, as current studies may face retraction as more information emerges.
20 Ultrasound Peripheral IV Education Initiative in the Emergency Department
Joseph Teresi, Jennalee Cizenski
SUNY Upstate Medical University
Objective: To increase number of indicated ultrasound IVs in the ED
Methods: We conducted a survey-based assessment for ED faculty at a level 1 academic center to identify barriers to performing ultrasound guided peripheral IVs. Ultrasound faculty/fellows implemented a standardized teaching approach using ultrasound machines and gel models resembling human tissue with underlying tubular structures representing peripheral veins. This educational intervention was available for two months both on shift in the ED and off shift at the department office building. Post-intervention surveys were sent out to assess the impact of the educational initiative.
Results: 79 residents and attendings responded to the pre-assessment and 50 responded to the post-assessment. For the 50 that completed both the pre and post survey there was no statistical difference in the response to how many PIV ultrasounds done (mean pre 2.55 and mean post 2.43). There was also not a statistically significant difference in impact of training (mean pre 2.92 and mean post 2.62). These were possibly due to a shorter time period between the educational intervention and the post-assessment compared to the pre-assessment. Despite the lack of statistical significance, however, we were able to identify important barriers to documenting and billing for US-guided PIVs, mostly related to the logistical/administrative aspect of recording US images and validating them in the software program QPath, which is separate from the main EMR system Epic.
Conclusion: The educational initiative implemented did not have a statistically significant impact on number of ultrasound PIVs performed post intervention when compared to pre-intervention. However, it is worth continuing to explore methods of teaching and promoting this important clinical skill. Furthermore, barriers to performing ultrasound PIVs, or at the very least documenting the procedure, were identified, and this warrants further investigation to identify and address these issues more specifically.
CASE REPORTS
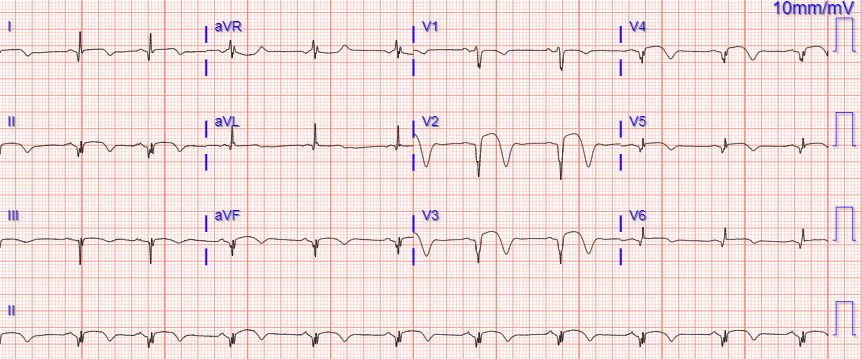
1 ECG Findings: That’s an Ugly ECG
Eli Johnson, DO. Nathan Weagraff, MD.
AdventHealth Emergency Medicine Residency, Orlando, Florida
A 79-year-old female with a medical history of myasthenia gravis, myocardial infarction (MI), aneurysm, and hypertension, was admitted to the emergency department (ED) following a fall. Despite the absence of chest pain, the initial electrocardiogram (ECG) obtained during transport by Emergency Medical Services (EMS) showed indications of a suspected ST-segment elevation myocardial infarction (STEMI). On arrival at the ED, the patient remained alert and oriented, reporting left leg pain and complaining of left lateral lower leg and lower back pain. Initial assessment in the ED revealed the patient’s baseline mental status, along with complaints of left leg pain. Further diagnostic workup, including laboratory tests and consultations, led to the identification of elevated troponin and N-terminal pro B-type natriuretic peptide (NT-proBNP) levels. Subsequent cardiac imaging revealed an akinetic portion of the left ventricle, prompting cardiac catheterization, which revealed a significant stenosis in the left anterior descending artery. The patient was managed with cardiac risk factor modification and ultimately discharged home.
2 Serotonin Syndrome Precipitated by Paxlovid Initiation
Nicholas Nasser, MD, Connor Welsh MD, Avir Mitra MD, Matthew Swan, MD
Mount Sinai Queens Emergency Medicine Residency Program
Throughout the COVID-19 pandemic, several antiviral medications have been studied for their effectiveness and safety in combating the novel pathogen SARS-CoV-2. Paxlovid, a combination of Nirmatrelvir and Ritonavir, came to market under Emergency Use Authorization (EUA) in December 2021 as a treatment for patients with mild-to-moderate coronavirus disease who are at high risk for progression to severe disease. In this case report, we will explore a case of a female in her early 40’s prescribed Paxlovid for a confirmed COVID-19 diagnosis who developed Serotonin Syndrome in the setting of concomitant use of agents including Buspirone, Quetiapine, and daily Kratom whose toxicity likely precipitated this effect.
Serotonin Syndrome is a rare and potentially lethal disorder characterized by excess serotonergic activity in the setting of serotonergic agent consumption. To date, there have been no reported cases of patients with COVID-19 taking Paxlovid presenting with Serotonin Syndrome. We conclude from this case report and literature review that more attention be made towards the potential drug interactions that can occur with the increased use of Paxlovid during the ongoing COVID-19 pandemic and future outbreaks. Clinicians should be mindful of the possibility of decreased elimination of serotonergic agents with Paxlovid initiation, and consideration should be made towards dose reduction of those agents or selection of other therapeutics to treat COVID-19 infection.
3 Abdominal Wall Hematoma in a High-Risk Patient: Navigating the Complexities of Anticoagulation
Arpita Gupta MD, Jeff Lapoint, DO
Kaiser Permanente San Diego Emergency Medicine
63-year-old male with hypertension, diabetes, chronic kidney disease, atrial fibrillation, and mitral regurgitation with mitral valve replacement on Coumadin presented with right lower abdominal pain that began one week ago after his last Lovenox injection following a recent TIA in the setting of subtherapeutic INR.
Abdominal exam revealed tenderness in the right lower quadrant without peritonitis. CT scan showed a hematoma in the right lower abdominal wall, measuring 13.5 cm by 8.5 cm by 18.5 cm with suspicion for active contrast extravasation. BMI stable at 34.9.
Hypotension and hemoglobin of 7.7 prompted transfusion of 2 units of packed RBCs, 2 units of FFP, and vitamin K followed by embolization by interventional radiology. On day 6, the patient’s hemoglobin dropped to 6.2 and a repeat CT scan revealed an expanding hematoma. He underwent a second embolization on day 7. The patient remained hemodynamically stable and was safely discharged on day 11.
In this case, the addition of a second anticoagulation agent should be done with caution and entail a detailed evaluation of risk and benefits. Older age, use of anticoagulation agents, and obesity predispose to the development of dangerous abdominal wall hematomas with possibly fatal consequences due to increased bleeding risk and different vascular structure and matrix composition of subcutaneous tissue [1]. Hemodynamic instability secondary to an abdominal wall hematoma is especially concerning for patients with multiple comorbidities who are poor candidates for surgical intervention. Relevant literature shows that mortality rates can range from four to twenty percent and conservative management is preferred for those with multiple chronic conditions given no increase in hematoma size and hemodynamic stability [2]. Careful consideration of anticoagulation regimens in patients with abdominal wall hematoma involving known risk factors, co-existing medical conditions, and early intervention can prevent sequelae, such as hemodynamic instability and fatality.
4 Dyspareunia as a Symptom of Urinary Tract infection
Milo Obas, BS, EMT, Dominguez Alberto Bali MD, PhD, Rochell Santana BS, Sodjinin R. Kassa RN-BSN
American University of Antigua College of Medicine
Background
UTIs often go undiagnosed due to clinicians prioritizing urinalysis over symptom evaluation. Consequently, dyspareunia, a common UTI symptom in women, is frequently overlooked during assessments, along with other typical UTI symptoms.
Methods
Retrospective review of 5500 patient charts (ages 17 to 72) were reviewed in our study from the Miami Center for Obstetrics Gynecology and Human Sexuality between 2007 and 2022.
Results
In 83% of the UTI cases studied over this time, dyspareunia was endorsed as a symptom. Approximately 94% of cases responded positively to treatment with antibiotics (Amoxicillin/Clavulanic acid or Nitrofurantoin). In post-menopausal women, the addition of local vaginal estrogen was necessary in around 45% of the cases with UTI, secondary to hypoestrogenism. We also found that 80% of women of reproductive age presenting with complaints of dyspareunia had an undiagnosed UTI.
Conclusion
While dyspareunia has been recognized as a symptom of interstitial cystitis, it has not been identified as a significant symptom of regular uncomplicated or complicated UTIs. These findings demonstrate that dyspareunia is an important aspect of the symptomatology of UTIs and is present alongside the classical symptoms such as dysuria, urodynia, pollakiuria, urgency, nocturia, and fever. Clinicians should consider UTI as a differential even when conventional tests are inconclusive.
5 Comparison of Survival and Sequelae following prehospital arrest and the use of Hydroxocobalamin
Joseph D Heath, Dr. Joan Dolinak
Upstate University Hospital, Syracuse, NY
Cyanide poisoning is a common cause of morbidity and mortality in house/structure fires. Hydroxocobalamin can be used as an effective antidote without side effects common to other cyanide antidotes. Hydroxocobalamin, common brand being Cyanokit, is safe for administration by prehospital staff and patients may in fact benefit from receiving it early in their care. We hypothesize that treating cyanide poisoning via early administration of hydroxocobalamin can help prevent cardiac arrest and improve potential for return of spontaneous circulation, ultimately increasing survival rate.
We performed a retroactive study to evaluate survival of patients involved in house fires that experienced cardiac arrest and received hydroxocobalamin. Using IMT assistance we collected information regarding administration of hydroxocobalamin in the hospital. Records of patients who received hydroxocobalamin were evaluated to determine if they experienced cardiac arrest and their final disposition from the hospital.
Out of a pool of 63 patients who had hydroxocobalamin ordered from 2014-2022 47 were found to be related to smoke inhalation/structure fire. Of these patients 41 received the medication, the remaining six had the medication ordered but not given; the order was cancelled, or the patient died/was made comfort measures only prior to administration. We found that patients were receiving hydroxocobalamin at roughly equivalent rates regardless of presence of cardiac arrest. These differences were not statistically significant (p=0.42).
Our goal was to look at the survival of prehospital cardiac arrest patients who received hydroxocobalamin. In our sample nearly half did not experience cardiac arrest. There were 15 prehospital arrests reported in the patients that received hydroxocobalamin. The nature of our data collection and chart review made it difficult to establish a chronological relationship between the time of arrest and the administration of hydroxocobalamin. Overall, there was no difference in survival between patients receiving hydroxocobalamin and not receiving hydroxocobalamin (p=0.67).
6 The Clot Traveled…Where?
Kiran Akbani, DO, Kimberly Buffkin, MD
AdventHealth Emergency Medicine Residency, Orlando, Florida
Introduction
It is well known that one of the most consequential and serious adverse effects of atrial fibrillation is thromboembolism, with the risk substantially higher in those who are not anticoagulated. Often, these emboli can travel to vital organs, with stroke being the most common embolic complication [1]. However, less commonly, these emboli can also travel
to an extremity, causing a sudden decrease in perfusion of the limb and creating a high risk of acute arterial ischemia.
Case report
We present the case of an elderly female with a known history of atrial fibrillation who presented with a chief complaint of right arm pain for the past few hours. She described the pain as traveling from her forearm down to her fingers. She admitted to non-compliance with her anticoagulation medicine. In the Emergency Department, she was accompanied by her family, who stated they believe the last time the patient took a dose of her Xarelto was 3 days prior, but they could not say for 100% certainty and stated it may be longer than that. The patient denied any prior history of blood clots or peripheral vascular disease. On physical exam, the left upper extremity had strong palpable brachial, radial, and ulnar pulses with strong grip strength and intact sensation of the entire extremity. By contrast, the right upper extremity had no palpable brachial, radial, or ulnar pulses. Doppler was also used, and no pulses were audible via Doppler distal to the antecubital fossa. The right upper extremity also had decreased grip strength and diminished sensation distal to the forearm when compared to the left upper extremity. Given the high concern for acute arterial ischemia secondary to emboli, vascular surgery was immediately consulted. The patient received a stat CT angiogram of the right upper extremity and was started on heparin and emergently transferred to a hospital with vascular capabilities for emergent operative management. The CT angiogram results demonstrated apparent complete occlusion of the right brachial artery and downstream right upper extremity arteries. In the operating room, the patient was found to have an ischemic right upper extremity and a thrombectomy of the proximal brachial artery was performed. Large amounts of thrombus were removed until no further thrombus was found to be present. This resulted in good flow with a palpable right radial pulse with Doppler radial and ulnar pulses. The patient was then taken to PACU in hemodynamically stable condition.
Conclusion
While our patient suffered a less-common adverse effect of atrial fibrillation by having an acute embolic event to the extremity rather than to her brain at the time of presentation, the same principles of anticoagulation recommendation apply, evident by her prescribed home medication of oral anticoagulation, but being non-adherent to it.
7 Well That Just Doesn’t Look Right: A Podiatric Anomaly
Tyler Littmann DO, Joshua Treimer DPM, Raluca Dima DPM, Clifford Denney, MD
AdventHealth Emergency Medicine Residency, Orlando, Florida
Case report
A 21-year-old otherwise healthy male presented to the ED approximately 2 hours after sustaining an injury to his right ankle while playing basketball. He was jumping up and landed incorrectly. He did not sustain any other injuries and denied any preceding symptoms prior to the injury. Differential diagnoses included ankle sprain, fracture, dislocation, compartment syndrome, and vascular injury. Plain radiographs confirmed a subtalar dislocation. Subtalar dislocations comprise only 1% of ankle dislocations. Following adequate analgesia, the reduction was achieved by flexing the knee to unlock the gastrocnemius and applying counter traction. The calcaneus was distracted with the non-dominant hand. The dominant hand plantarflexed and distracted the forefoot. The patient was discharged home with strict non-weight bearing instructions and orthopedic follow-up.