Background
COVID-19 is associated with severe respiratory illness,1–4 ischemic strokes, subarachnoid hemorrhage5 coagulopathic events,6,7 threatened miscarriage,8 and other serious pathologies. It is also associated with relatively benign infection.9 Front-line workers such as emergency medical personnel (EMS) are especially prone to infection, as they are the ones who interact when the patient is in extremis, and may not have the benefit of strict airborne precautions during transport. Many EMS workers experience anxiety about getting sick with COVID-19 themselves, and also about being asymptomatic carriers and infecting their loved ones. Both these scenarios would be alleviated by having access to COVID-19 testing.
There are two types of tests for COVID-19. The diagnostic (molecular) test to detect active infection is a nucleic acid polymerase chain reaction (PCR) assay obtained via a nasopharyngeal swab. Accuracy is hampered by improperly performing the test; the swab must be from the nasopharynx and not the oropharynx, as saliva will dilute the sample. It is ideally done after the onset of infection when viral load is highest but patient may already be symptomatic, so it could be “too late” to help prevent spread. The overall sensitivity is currently only 60-70%.10 The antibody (serologic) test is used to detect evidence of past infection. These tests can detect IgM antibody (marker of early infection) or IgG (marker of late infection) or both. Test is ideally performed 3 days-3 weeks after the infection has resolved. Presumably the presence of these antibodies confer immunity, but we do not yet know how long this immunity lasts.11 Thus, it is possible that a person can get a subsequent COVID-19 infection after having previously recovered from one. A combination of diagnostic and serologic tests may give the best picture, since we do not exactly know when infection begins.
We hypothesized that our front-line workers, in particular emergency medical services (EMS) personnel (paramedic team) have all had COVID-19 exposure sometime over the last few months of caring for them. This exposure caused a lot of worry for EMS, many of whom opted to live apart from their families early in the pandemic due to fear they would infect them. However, there is evidence that many may be asymptomatic carriers, so it is entirely possible that EMS personnel, who are largely young healthy folk, had already been infected, already exposed their families, and everyone had convalesced. The only way to know this is to do antibody testing.
Serologic antibody tests measure two types of antibodies, IgM and IgG.12 IgM is considered an early marker of convalescence while IgG is associated with long term immunity.
The objective of this study was to perform COVID-19 diagnostic and serologic testing on emergency medical personnel in Polk County to determine: 1) COVID-19 prevalence 2) Rate of convalesced personnel (+antibodies) and 3) Rate of asymptomatic carriers
Methods
This clinical trial (NCT04682132) ) was registered at clinicaltrials.gov, a resource provided by the U.S. National Library of Medicine. It was conducted at Polk County Fire Rescue (PCFR), one of the largest EMS systems in the state of Florida. PCFR responds to over 115,000 calls per year and covers a geographic area of over 2000 square miles. The study assessed COVID-19 antibody status in PCFR medics and correlated antibody status to 1) symptomatology, 2) amount of patient contact and 3) individual co-morbidities. For symptoms survey, medics were given a QR code to a survey prior to antibody testing. Approval was granted by the Institutional Review Board of the University of Central Florida, study ID#00001784.
Results
The median age of the cohort (N=409) was 43 years (IQR 33-52). 41% were female. 83% were White, 9% were Black, 1% were Asian, and 6% were other. Twelve percent were Hispanic. Thirty-three percent had the following co-morbidities: 5% diabetes, 6% asthma, or chronic obstructive pulmonary disease. 17% had hypertension. Forty-five percent had received their influenza vaccine. The median body mass index (BMI) was 19.8 (IQR 25.9-34.8 ). Nineteen percent were symptomatic. The most common symptoms were cough, fatigue, and headache. Almost 40% had direct patient contact. Fifteen percent had less than 5 hours of patient contact per week; 27% had 5-20 hours per week, and 57% had more than 20 hours per week of direct patient contact.
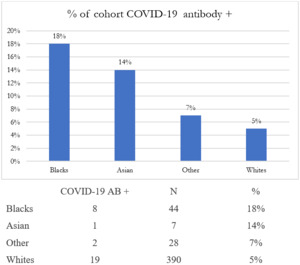
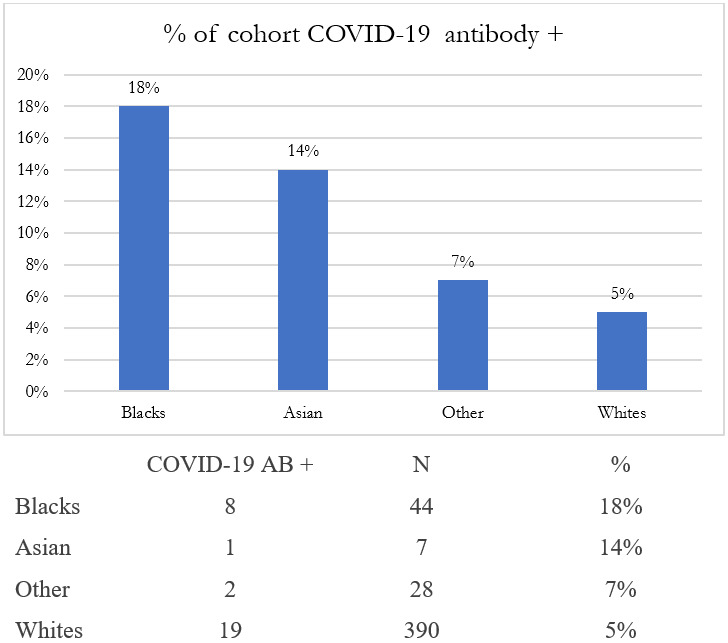
A total of 7% had a positive COVID-19 antibody test. The racial breakdown of COVID-19 positivity by race is depicted in Figure 1. Although Black EMS personnel only comprised 9% of the cohort, they comprised 18% of those who tested positive for COVID-19. The only univariate analysis that was statistically significant for antibody status was race. Black EMS personnel had 3.94 times the odds of having a positive COVID-19 antibody compared to Whites. (P=0.0012 Pearson correlation, 95%CI 0.0560 – 0.2248).
Black race remained a statistically significant predictor in a multivariate model that included the age, sex, BMI, number of hours of direct patient contact, whether the medic was symptomatic, presence of co-morbidities and whether or not the medic had received a flu shot prior was symptomatic (P=0.0008, 95% CI 0.0621-0.2354).
Discussion
The COVID-19 positivity rate refers to the percentage of people who test positive for the virus out of all those who have been tested.13 It is an important metric to understand the spread of the virus in different communities and populations. When discussing the COVID-19 positivity rate in Black and other marginalized communities, it is crucial to consider various factors such as socio-economic status, access to healthcare, and underlying health conditions, which can significantly impact the rate of positivity.14 Several studies and reports have indicated that Black communities have experienced higher positivity rates compared to other racial and ethnic groups .15 This could be due to a variety of factors including higher exposure risk, limited access to testing, and pre-existing health conditions. Pre-existing health conditions such as hypertension, diabetes, and obesity are more prevalent in Black communities. These conditions can increase the severity of COVID-19 symptoms and may contribute to higher positivity rates. Socio-economic factors such as income, employment, and housing conditions play a significant role in determining the risk of exposure to the virus. Black communities often face socio-economic disparities, leading to higher exposure risk and consequently higher positivity rates.
Access to testing is a significant factor affecting positivity rates. Communities with limited access to testing services may have higher positivity rates as individuals may only get tested when they exhibit severe symptoms.16
Vaccination rates are also an important factor to consider.17 A survey of 58 Black residents in Brooklyn, New York, showed that unvaccinated Black non-Hispanic respondents report significant concerns about vaccine safety and efficacy and have greater mistrust in the vaccine development process.18 Lower vaccination rates in Black communities can lead to higher positivity rates as the population remains more susceptible to the virus. The effectiveness of public health interventions like social distancing, mask mandates, and lockdowns can also impact positivity rates in different communities. Knowledge of the COVID-19 virus is also connected to whether individuals get the vaccine.19 Raising awareness and providing education about preventive measures, testing, and vaccination is crucial in reducing positivity rates in Black communities. Accurate and comprehensive data collection and reporting are essential for understanding the true extent of positivity rates in different communities and for developing targeted interventions.
Conclusion
In a cohort of paramedics actively managing patients, the COVID-19 positivity rate was significantly higher for Blacks compared to whites.