Introduction
Endosalpingiosis, defined as the presence of fallopian tube-type epithelium outside its usual location, has been reported in various ectopic sites but remains exceedingly rare in the urinary bladder. The aetiology and clinical behaviour of this condition are not fully understood. Histological examination, often supplemented by immunohistochemistry, remains the cornerstone of diagnosis. Here, we present a rare case of urinary bladder endosalpingiosis and discuss its clinical, radiological, and histological features in the context of the existing literature.
Case Report
A 58-year-old multiparous woman (para 3) was referred to the urology clinic with a five-month history of recurrent culture-positive urinary tract infections associated with intermittent macroscopic haematuria, with each episode resolving following antibiotic therapy. Flexible cystoscopy revealed a 0.5–1 cm papillary lesion on the posterior bladder wall near the dome, and she was scheduled for a contrast-enhanced CT and cystoscopy with transurethral resection (TURBT) of bladder tumour.
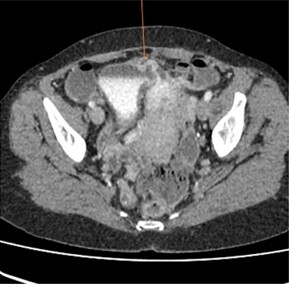
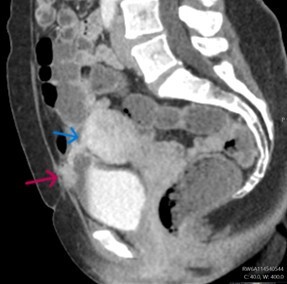
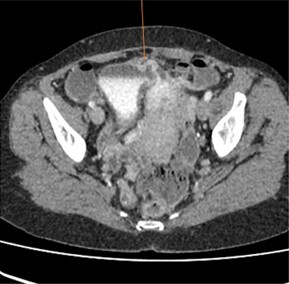
A contrast-enhanced CT scan (Figures 1 & 2) revealed a bladder tethered to the uterus with a diverticulum exhibiting irregular wall thickening and enhancement along its anterior-superior aspect. Subsequently, a 0.5 g bladder tissue, including the lesional area was resected during TURBT procedure. Her past medical history includes three caesarean sections, one complicated by an incidental bladder injury. She denies smoking, occupational chemical exposure, pelvic radiotherapy, chronic catheter use, anticoagulant therapy, nephrolithiasis apart from the noted calculus, recurrent gross haematuria outside infection or systemic diseases and there is no family history of urological malignancy.
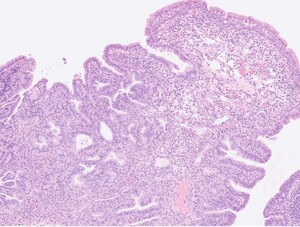
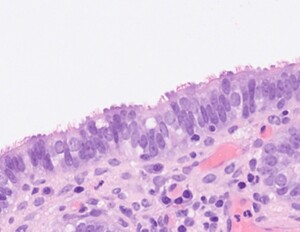
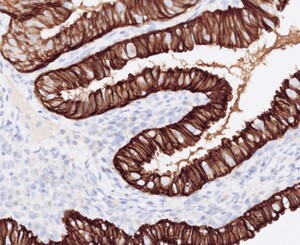
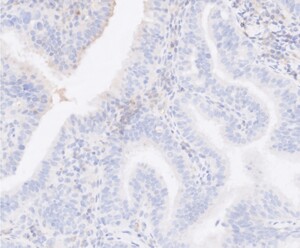
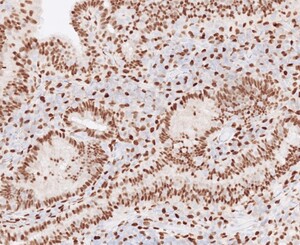
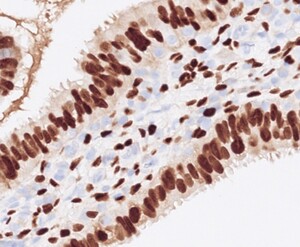
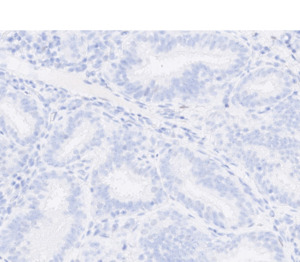
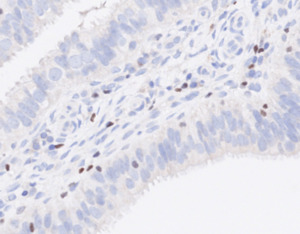
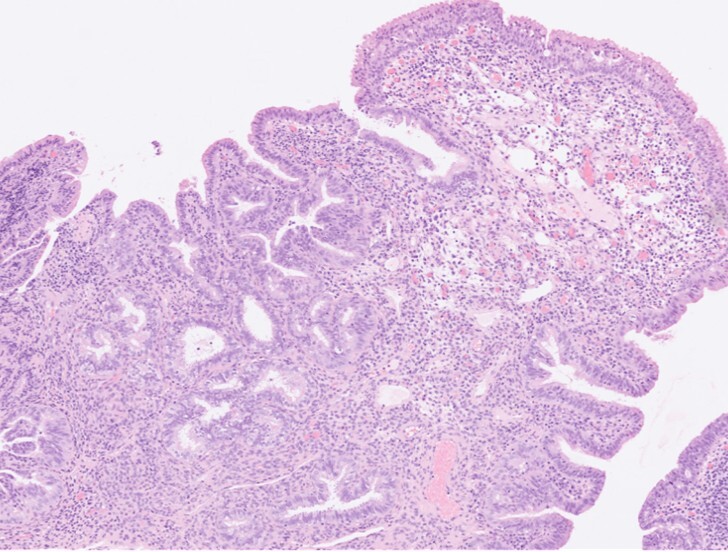
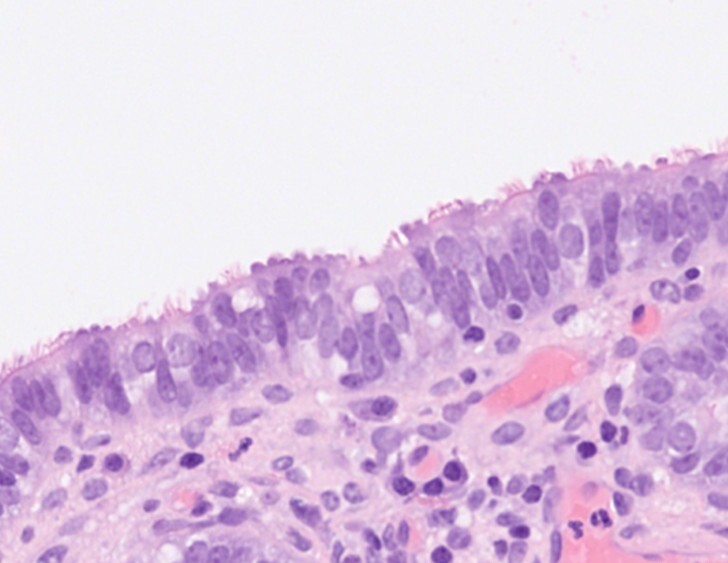
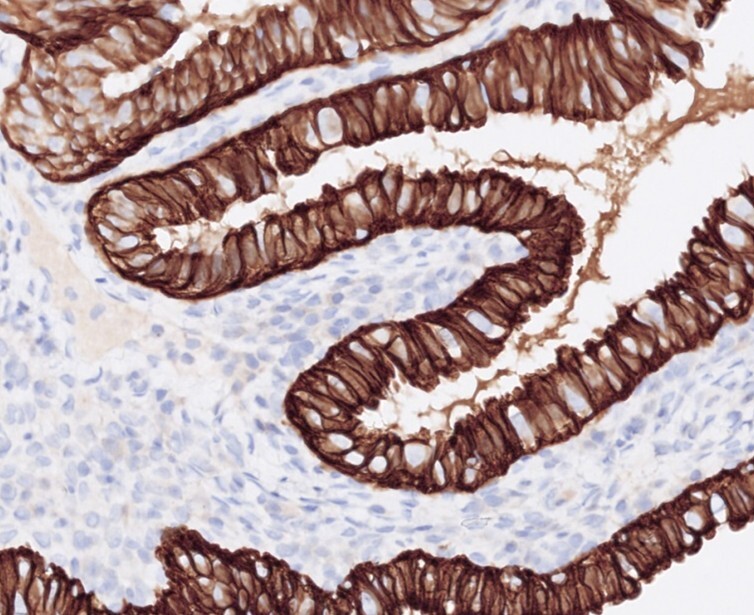
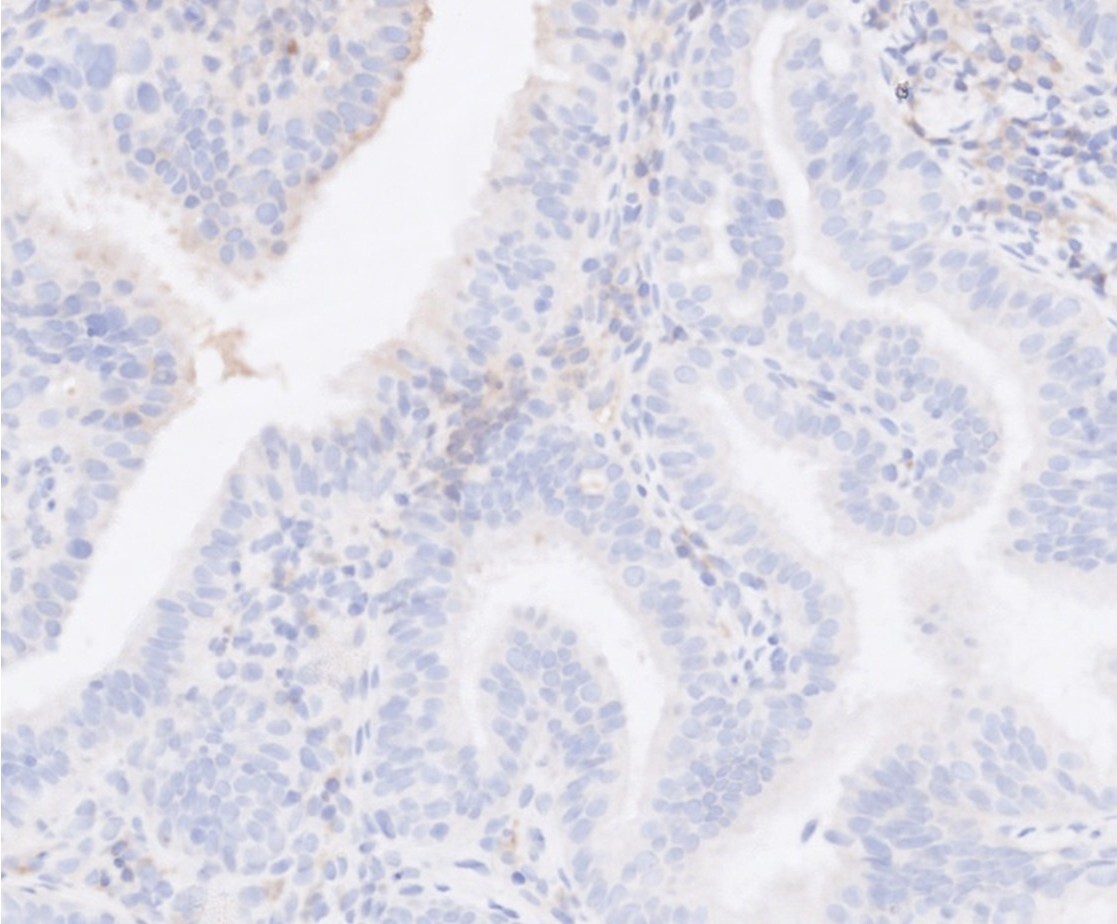
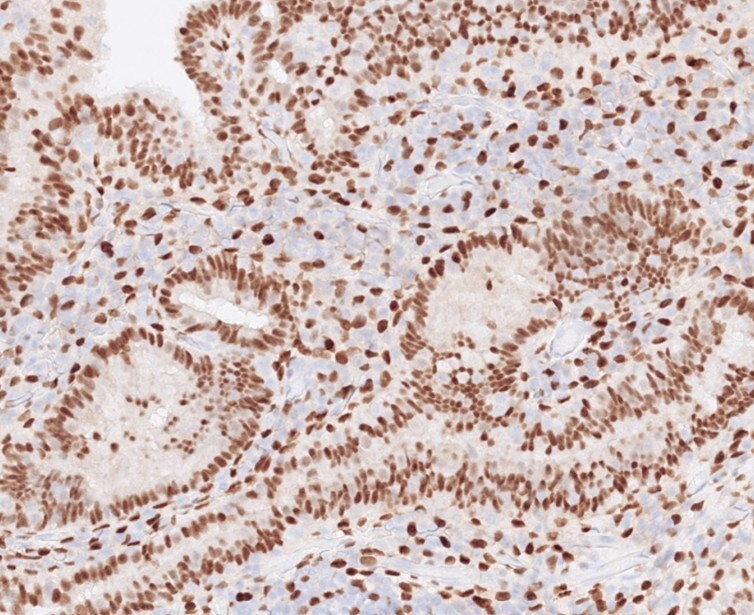
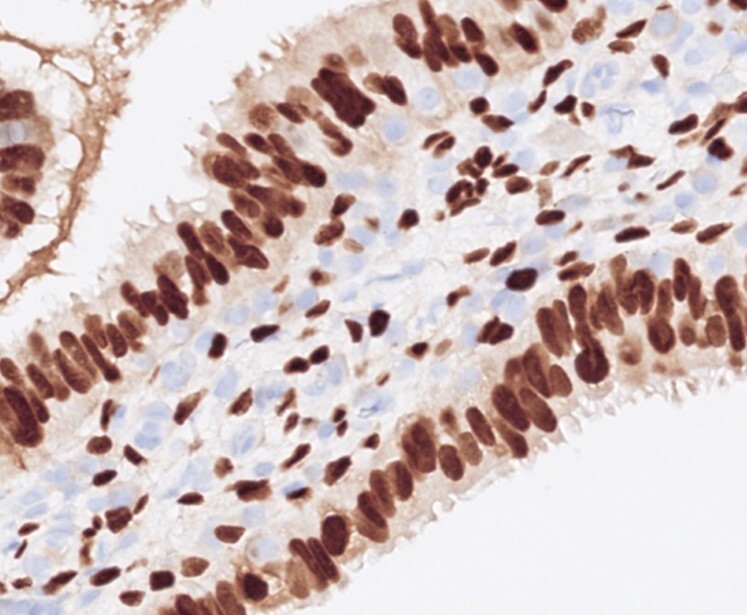
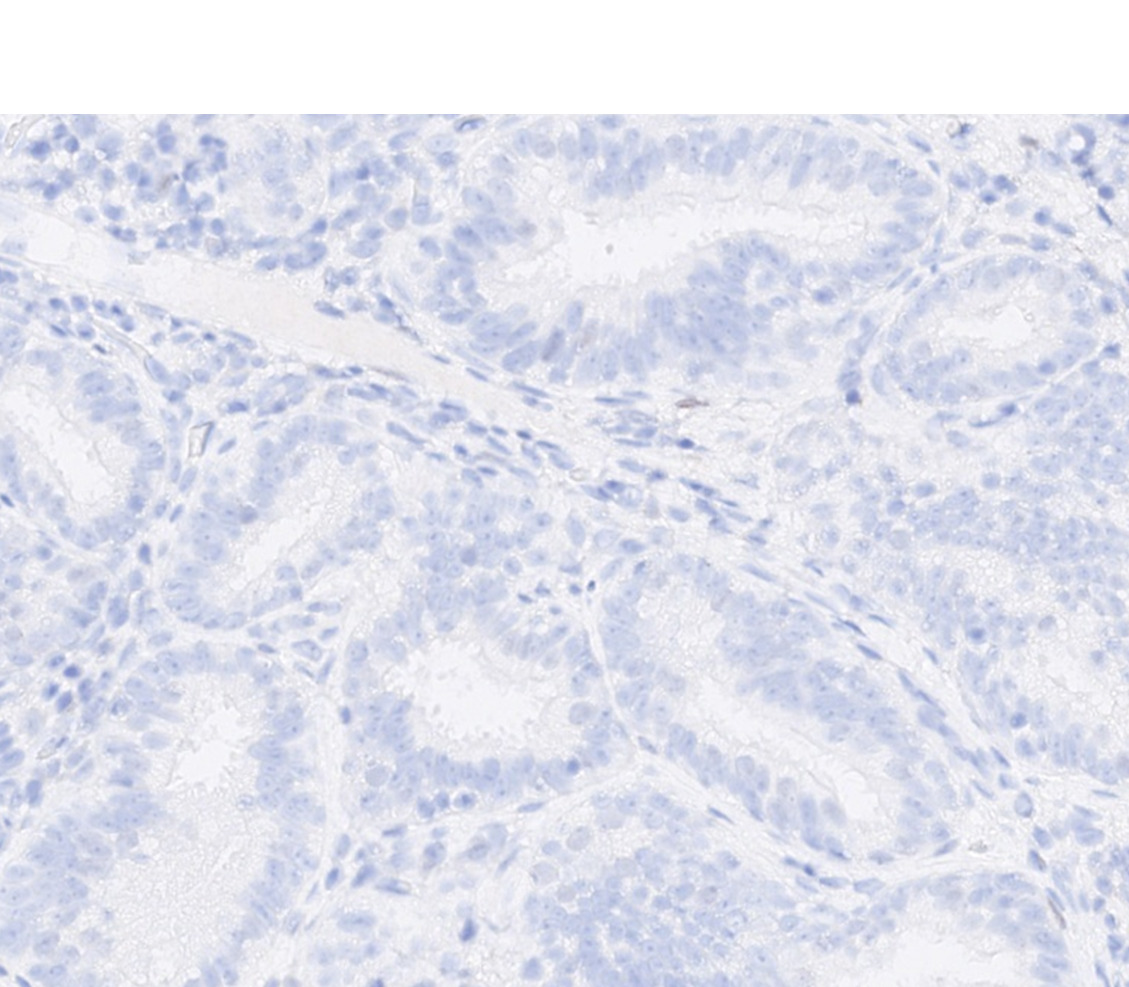
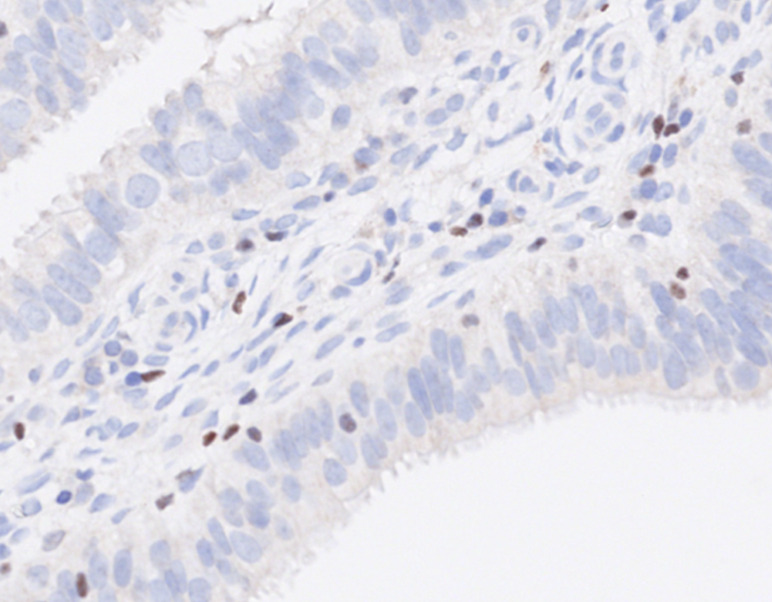
Histopathological examination (Figures 3 & 4) showed polypoid mucosal changes with papillary projections and cystic, dilated tubules lined by fallopian tube-type epithelium. No nuclear atypia, increased mitoses, or other Mullerian elements such as endocervical or endometrial tissue were identified. Immunohistochemistry (Figures 5-10) demonstrated positivity for CK7, oestrogen receptor, and progesterone receptor, while GATA3, P63, and CK20 were negative.
Based on these findings, a diagnosis of urinary bladder endosalpingiosis was made. Follow-up cystoscopy and biopsy after three months showed mild chronic inflammation without residual or recurrent endosalpingiosis. She was commenced on a prophylactic antibiotic for 3–6-month duration, and urological standpoint, it was determined that routine long-term follow-up was not required.
Discussion
Endosalpingiosis of the urinary bladder is a very rare entity characterized by the presence of fallopian tube-type epithelium in the urinary bladder. The term endosalpingiosis was first described by Sampson in 1930. Endosalpingiosis has been reported in many ectopic sites, like pelvic organs, pouch of Douglas, omentum, bowel serosa, skin, lymph nodes, and periaortic area. Only a limited number of cases of urinary bladder endosalpingiosis have been found in the English literature, making it a challenging diagnosis,1–8 and most have occurred as part of Müllerinosis, where endosalpingiosis coexists with endometriosis and/or endocervicosis. In contrast, isolated endosalpingiosis of the bladder, as seen in our patient, remains distinctly uncommon.
Clinical presentation can be variable, ranging from asymptomatic or incidental finding to alarming symptoms such as dysuria, haematuria, abdominal or pelvic pain. The age range of the patients spans from 34 to 68 years in the reported cases.
Radiological findings are often nonspecific, making pre-operative diagnosis challenging. Histological examination is essential for confirmation. It reveals tubal or papillary structures lined by characteristic fallopian tube-type epithelium with three types of cells, which include ciliated cells, mucinous cells, and intercalated cells, located in the lamina propria or muscularis propria of the urinary bladder wall. Immunohistochemistry findings are identical to the fallopian tube with CK7, oestrogen, and progesterone receptor positivity and absence of urothelial markers like GATA3, uroplakin II, uroplakin III and P63.
It is important to differentiate endosalpingiosis from other benign and malignant conditions that can mimic its appearance macroscopically and microscopically. Differential diagnosis in histology includes cystitis glandularis, nephrogenic adenoma, urachal remnants, and adenocarcinoma of the urinary bladder. Immunohistochemistry is a valuable tool in establishing the diagnosis in problematic cases, especially when the fallopian tube-type epithelial elements extends to the muscularis propria mimicking an invasive carcinoma.
The exact aetiology of the endosalpingiosis remains unclear. Two primary hypotheses have been proposed: the metaplastic theory and implantation theory. Metaplastic theory suggests that fallopian tube-type epithelium arises from metaplasia of the remaining transitional epithelium of the urinary bladder. The implantation theory postulates that tubal tissue is transported to the site during surgical manipulation, where it implants and grows. Many of the patients with urinary bladder endosalpingiosis have a history of gynaecological or pelvic surgery,1–3 which supports the implantation hypothesis.
In contrast to Müllerinosis cases—often reported in patients without prior surgical trauma and thought to arise via metaplastic mechanisms—our patient had a history of two caesarean sections and a documented intraoperative bladder injury. This clinical background strongly implicates implantation as a plausible mechanism, distinguishing this case from metaplasia-associated or co-occurrence lesions and adding weight to the argument that surgical disruption may facilitate epithelial seeding into the bladder wall.
Surgical excision of the lesion has been performed in many patients as the primary treatment. Recurrences have not been reported to date, including this patient, whose follow-up studies did not show recurrence or residual disease.
Endosalpingiosis elsewhere, like in the ovary, has been described in co-occurrence with tumours such as ovarian borderline tumours, serous, endometrioid, and clear cell carcinoma of the ovary. This shows a similar distribution pattern to endometriosis and ovarian malignancies. Only a single case report has suggested an association with endosalpingiosis and malignancies in the urinary bladder.9 It has described a clear cell adenocarcinoma of the urinary bladder in an area of endosalpingiosis. As the reported cases are limited, more data are required to determine the premalignant nature of the condition.
Summary
Endosalpingiosis of the urinary bladder is a rare condition with variable clinical presentations and surgical history, radiological correlation, and histological examination are crucial for diagnosis. This case differs from most published reports by presenting as isolated bladder endosalpingiosis in a patient with clear surgical risk factors, thereby supporting an implantation-related pathogenesis. Further research is needed to understand the clinical behaviour and long-term outcome of the condition.
Acknowledgements
The authors extend their gratitude to Zosia Rodak, Consultant Radiologist, Department of Radiology, Northern Care Alliance NHS Foundation Trust, for her assistance with radiological imaging.