Introduction
Choledocholithiasis, or the presence of common bile duct (CBD) stones, remains a significant clinical problem encountered in 10–20% of patients with gallbladder stones.1 These stones can lead to serious complications such as obstructive jaundice, cholangitis, and pancreatitis, making prompt diagnosis and effective management crucial.2
Over the past decades, two primary management strategies have evolved: the two-stage approach, involving preoperative endoscopic retrograde cholangiopancreatography (ERCP) followed by laparoscopic cholecystectomy (LC), and the single-stage approach, which combines laparoscopic CBD exploration (LCBDE) with LC in one procedure.3 While ERCP has been considered the standard in many centers, the single-stage laparoscopic approach has gained attention due to advancements in minimally invasive surgery and increasing expertise among surgeons.4
Proponents of the one-stage approach argue that it offers several potential advantages, including reduced hospital stay, fewer anesthesia exposures, and lower overall costs, while achieving comparable stone clearance rates.5 However, critics highlight the technical challenges, the need for specialized equipment and training, and the risk of bile duct injury or incomplete clearance.6,7 Therefore, determining which approach provides superior outcomes in terms of efficacy, safety, and recovery remains a topic of active investigation.
This study aims to compare the clinical outcomes, safety profile, and postoperative recovery between one-stage laparoscopic management (LCBDE with LC) and the conventional two-stage approach (ERCP followed by LC) in patients with gallbladder and CBD stones.
Methods
Study design and setting
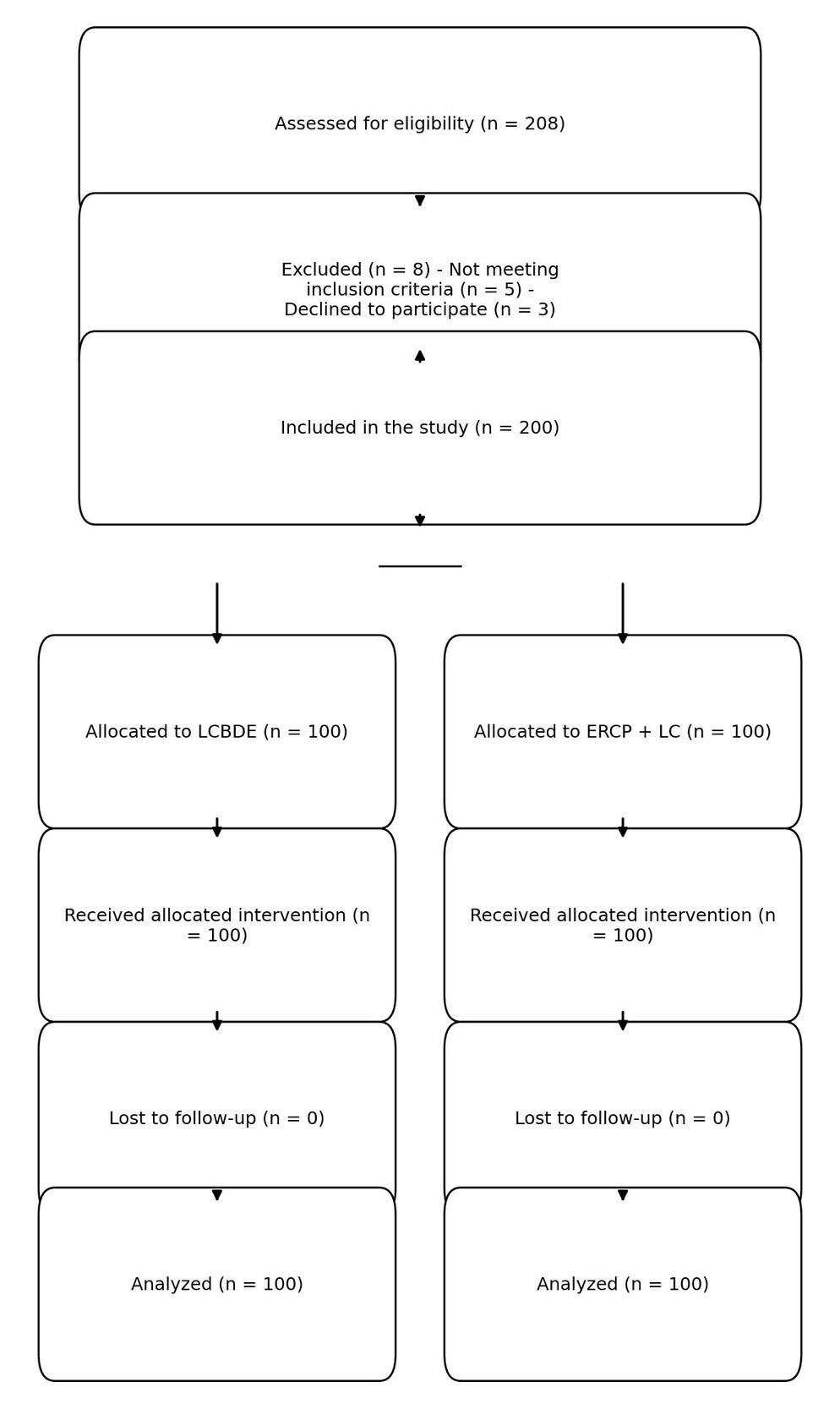
This was a prospective randomized comparative study conducted at Sohag University Hospital, Faculty of Medicine, Sohag University, Egypt, between January 2018 and December 2024. A total of 208 patients with concurrent gallbladder and common bile duct (CBD) stones were assessed for eligibility, 8 were excluded prior to randomization (5 did not meet inclusion criteria and 3 declined participation). The remaining 200 patients were randomly assigned to either the LCBDE group or the ERCP followed by LC group using a computer-generated randomization sequence in a 1:1 allocation ratio. Randomization was concealed in sealed opaque envelopes, and allocation occurred after eligibility confirmation. The study flow and patient allocation process are illustrated in Figure 1.
Sample size calculation
The sample size was determined a priori based on detecting a clinically relevant difference of 1.5 days in hospital stay between groups, assuming a standard deviation of 3 days, α = 0.05, and power (1–β) = 0.80. This required a minimum of 90 patients per group. To account for potential dropouts, 100 patients were enrolled in each arm.
Ethical Approval
The study protocol was approved by the Medical Research Ethics Committee (MREC) of the Faculty of Medicine, Sohag University (Approval No: SUV-MED-REC-2018-0317; Date: January 15, 2018). The research was conducted in accordance with the ethical standards of the Declaration of Helsinki and written informed consent was obtained from all participants prior to enrollment.
Patient selection and preoperative assessment
Inclusion criteria were age 18–80 years and confirmed concomitant gallbladder and CBD stones on preoperative magnetic resonance cholangiopancreatography (MRCP) or demonstration of stones on intraoperative cholangiography. Exclusion criteria included prior biliary surgery, intrahepatic stones, hemodynamic instability or acute ascending cholangitis necessitating urgent ERCP, and American Society of Anesthesiologists (ASA) physical status > III. Preoperative assessment comprised history and physical examination, laboratory testing (complete blood count, liver function tests, coagulation profile), abdominal ultrasound, MRCP and anesthetic risk evaluation.
Operative techniques and perioperative care
Procedures were performed by a team of consultant surgeons and endoscopists with comparable caseload. In the LCBDE group, standard four-port laparoscopic cholecystectomy was followed by CBD exploration via a transcystic approach when feasible; choledochotomy was employed for large or multiple stones. Stone extraction used Dormia baskets, balloon catheters or, selectively, lithotripsy. CBD closure was by primary duct closure or T-tube drainage according to intraoperative findings (primary closure in 70/85 applicable cases, T-tube in 15/85). Intraoperative cholangiography verified duct clearance. In the ERCP+LC group, ERCP with sphincterotomy and stone extraction was performed under fluoroscopic guidance; laparoscopic cholecystectomy was scheduled within 3–5 days thereafter. Standard anesthesia, perioperative antibiotics, DVT prophylaxis and analgesic protocols were applied to both groups.
Postoperative Care and Discharge Criteria
Postoperatively, all patients received standardized analgesia, early ambulation, and gradual reintroduction of oral intake. Laboratory and imaging evaluations were performed to assess biliary function and exclude retained stones.
Patients were discharged once they achieved full oral intake, adequate pain control with oral medications, no signs of bile leakage, and stable vital parameters for at least 24 hours.
Follow-up
All patients were followed for one year postoperatively. Follow-up visits were scheduled at 1 week, 1 month, 6 months, and 12 months. Each visit included clinical assessment, liver function tests, and ultrasonography. MRCP was performed selectively in cases with abnormal liver enzymes or biliary symptoms to detect retained or recurrent CBD stones. Patient satisfaction was reassessed at 3 months using a validated 5-point Likert scale.
Outcome Measures
The primary outcome was successful removal of both CBD stones and the gallbladder without conversion to alternative approaches. Successful stone clearance was defined as the complete removal of all CBD stones, confirmed intraoperatively by cholangiography or endoscopic visualization.
Secondary outcomes included operative time (minutes), intraoperative complications, conversion rate, postoperative pain (Visual Analogue Scale, 0–10) on postoperative days 1 and 3, length of hospital stay, postoperative complications (Clavien–Dindo grade ≥ II within 30 days), retained CBD stones (any stone detected by ultrasonography or MRCP within six months postoperatively), and patient satisfaction (5-point Likert scale at discharge and 3-month follow-up), Although a validated 5-point Likert scale was used to assess patient satisfaction, responses were subsequently grouped into three categories (1 = dissatisfied [scores 1–2], 2 = neutral [score 3], 3 = satisfied [scores 4–5]) for statistical clarity and comparability.
Statistical analysis
Data were analyzed using IBM SPSS Statistics version 28.0 (IBM Corp., Armonk, NY, USA). Quantitative variables were presented as mean ± standard deviation (SD) or median (interquartile range) depending on data distribution, and qualitative variables as frequency and percentage.
Comparisons between groups were performed using the Student’s t-test or Mann–Whitney U test for continuous variables, and the Chi-square test or Fisher’s exact test for categorical variables. Multivariate logistic regression analysis was conducted to identify independent predictors of success and complications. A p-value <0.05 was considered statistically significant.
Cost analysis
The cost analysis was performed using actual hospital-based data from Sohag University Hospital. Only direct medical costs were considered, including procedure-related expenses, anesthesia, hospital stay, and postoperative medications. Indirect costs (e.g., patient loss of income or travel expenses) were not included. The mean total cost per patient was calculated for each group, and presented as a percentage difference between groups. Cost data were analyzed using Student’s t-test or Mann–Whitney U test as appropriate.
Results
Between January 2018 and December 2024, 200 patients were enrolled and analyzed: 100 patients underwent single-stage laparoscopic common bile duct exploration with cholecystectomy (LCBDE group) and 100 patients underwent two-stage management with ERCP followed by laparoscopic cholecystectomy (ERCP + LC group). All patients completed the planned follow-up schedule (mean follow-up 12.6 ± 3.3 months).
Baseline demographic and clinical characteristics
Baseline characteristics were similar between groups (Table 1). Mean age was 49.8 ± 11.6 years in the LCBDE group versus 50.4 ± 12.2 years in the ERCP + LC group (p = 0.68). Sex distribution, BMI, history of previous abdominal surgery, and preoperative total and direct bilirubin levels did not differ significantly between groups (sex M/F 48/52 vs 46/54, p = 0.75; BMI 27.5 ± 3.8 vs 27.8 ± 4.0, p = 0.60; previous abdominal surgery 15% vs 18%, p = 0.55; total bilirubin 2.8 ± 1.5 mg/dL vs 3.1 ± 1.8 mg/dL, p = 0.18; direct bilirubin 2.3 ± 1.4 mg/dL vs 2.6 ± 1.6 mg/dL, p = 0.15).
Operative and hospitalization outcomes
Operative time was significantly shorter in the LCBDE group (142 ± 35 min) compared with the ERCP + LC group (288 ± 60 min; p < 0.001). Conversion to open surgery occurred in 4% of LCBDE cases and 6% of ERCP + LC cases (p = 0.50). Mean hospital length of stay was 6.0 ± 2.0 days for LCBDE and 6.5 ± 2.3 days for ERCP + LC; the difference did not reach statistical significance in univariate analysis (p = 0.20) (Table 2). However, in multivariate linear regression (Table 2), procedure type (ERCP) was independently associated with a prolonged hospital stay (+0.8 days; SE 0.3; p = 0.008), after adjustment for age, preoperative bilirubin, stone number, diabetes, and intraoperative complications.
Postoperative pain and recovery
At 24 hours, the proportion of patients reporting severe pain (VAS 8–10) was lower in the LCBDE group than in the ERCP + LC group (15% vs 25%, p = 0.01). By postoperative day 3, moderate pain (VAS 4–7) was less frequent in the LCBDE group (10% vs 20%, p = 0.02). Pain resolution rates were 85% for LCBDE and 78% for ERCP + LC (p = 0.20). Mean time to bilirubin normalization did not differ significantly between groups (3.2 ± 1.5 days vs 3.5 ± 1.8 days, p = 0.18) (Table 3).
Complications and success rates
Minor complications occurred in 5% of LCBDE patients and 7% of ERCP + LC patients (p = 0.55). Major complications were observed in 3% and 5% of patients, respectively (p = 0.47). There were no life-threatening complications in either group. Overall procedural success (complete stone clearance and cholecystectomy without conversion to alternative modalities) was 98% in the LCBDE group and 97% in the ERCP + LC group (p = 0.65). One-year stone recurrence rates were 2% versus 4% (p = 0.40) (Table 4).
Economic and long-term outcomes
Resource utilization differed markedly between strategies. LCBDE involved a single procedure per patient compared with two procedures per patient for ERCP + LC. Total operating room time averaged 142 minutes for LCBDE versus 288 minutes for the staged approach (+103% for ERCP + LC). Readmission rates and ICU admissions were higher in the ERCP group (readmission 6% vs 3%; ICU admissions reported in supplementary analysis). LCBDE was associated with a median cost reduction of 40% (95% CI: 35–50%) compared to the two-stage approach (p < 0.001) (Table 5). Mean follow-up duration was comparable (12.5 ± 3.2 vs 12.8 ± 3.5 months, NS). Patient satisfaction (1–3 scale) trended higher after LCBDE (2.5 ± 0.8 vs 2.3 ± 0.9; p = 0.08) but did not reach statistical significance, Although the difference in patient satisfaction did not reach statistical significance (p = 0.08), the observed trend may reflect a clinically meaningful preference for the single-stage approach, particularly in the context of reduced postoperative pain and streamlined care.
Detailed and multivariate analyses
Stone characteristics and laboratory profiles are presented in Tables 6 and 7; no significant between-group differences were found in stone size distribution or CBD diameter. Technical variations and extraction methods are detailed in Table 8. Multivariate linear regression for length of hospital stay identified the following independent predictors of prolonged stay: procedure type (ERCP) +0.8 days (SE 0.3; p = 0.008), age per 10-year increment +0.5 days (SE 0.2; p = 0.01), preoperative bilirubin >4 mg/dL +1.2 days (SE 0.4; p = 0.003), multiple stones +0.7 days (SE 0.3; p = 0.02), intraoperative complications +2.1 days (SE 0.6; p = 0.001), and diabetes +0.6 days (SE 0.3; p = 0.04). Post-hoc power analysis (Table 9) indicated adequate power (~85%) to detect the observed difference in length of stay.
Discussion
In this prospective comparative series of 200 patients, single-stage laparoscopic common bile duct exploration (LCBDE) combined with laparoscopic cholecystectomy demonstrated clinical performance at least equivalent to the classic two-stage ERCP + LC strategy for duct clearance, while offering advantages in early patient-centered outcomes (lower early postoperative pain), resource utilization (fewer procedures and markedly lower total OR time), and estimated cost.8
Length of stay and economic impact were important differentiators in our cohort. Although the observed mean hospital stay was shorter after LCBDE, this difference did not reach statistical significance in the univariate comparison (p = 0.20). Nevertheless, multivariate modeling showed that procedure type (ERCP) independently predicted a longer length of stay (+0.8 days; p = 0.008), suggesting that when adjusting for confounders the staged approach is associated with prolonged hospitalization. Therefore, while unadjusted comparisons indicate only a trend, adjusted analyses support an effect of the treatment pathway on hospital resource use. These findings align with recent institutional and multicenter analyses that found shorter admissions and significantly lower hospital charges with LCBDE, supporting its viability as a cost-saving alternative in appropriate settings.9
Our cost and patient-centered analyses together highlight the broader value of the single-stage approach. The LCBDE pathway was substantially less expensive than the two-stage ERCP + LC strategy, primarily due to shorter total hospital stay and the avoidance of duplicate anesthesia and admissions. Moreover, patients undergoing the single-stage procedure reported significantly less pain at 24 hours and day 3, with a trend toward higher satisfaction (p = 0.08). Although indirect costs (e.g., time off work, repeated anesthesia, and dual admissions) and detailed quality-of-life data were not formally included, these findings suggest that the one-stage pathway not only reduces direct hospital expenditures but also likely improves early recovery experience and overall patient-perceived value. This integration of cost efficiency with patient comfort underscores the multidimensional advantage of the single-stage strategy.10
Operative time comparisons in the literature are mixed. Some reports describe longer total theatre time for one-stage LCBDE (when the entire single procedure is compared to a single component of the staged pathway), while others show parity or shorter aggregate OR time when the staged ERCP and LC are combined. In our cohort the aggregate operating-room time markedly favored the single-stage strategy, consistent with studies that account for the cumulative resource use of staged care.11 These differences highlight the importance of reporting aggregate rather than per-procedure metrics when comparing pathways.12
Safety remains central to any recommendation. We observed low rates of major complications (3% vs 5%) and no life-threatening events, comparable to contemporary series demonstrating similar morbidity profiles between approaches when performed by experienced teams.13 Notably, ERCP carries a specific risk of post-ERCP pancreatitis and procedure-related complications that may increase readmissions and extend hospitalization; conversely, LCBDE requires surgical instrumentation and technique (transcystic vs choledochotomy, primary closure vs T-tube) that demand operative skill and institutional resources.14 Our multivariate analysis confirms that intraoperative complications and higher preoperative bilirubin are strong predictors of prolonged stay, reinforcing the principle of individual patient selection.15
Although patient satisfaction trended higher after LCBDE (p = 0.08) and did not achieve formal statistical significance, this result may represent a clinically relevant trend that warrants confirmation in larger multicenter studies.
Practical implications: For centers with adequate laparoscopic hepatobiliary experience and equipment, a one-stage LCBDE pathway can streamline care — reducing the number of anesthetic events, cumulative OR time, and likely cost — while maintaining high clearance and acceptable safety. For patients with high operative risk, complex anatomy, or where local endoscopic expertise is stronger than surgical biliary experience, the staged ERCP approach remains valuable.
Clinical applicability: These findings may inform surgical decision-making in tertiary centers where laparoscopic expertise and infrastructure are available, promoting efficient, patient-centered, and cost-effective management of concomitant gallbladder and CBD stones.
Our findings derive from a single high-volume tertiary center where surgeons had substantial experience in LCBDE. Therefore, caution is warranted when extrapolating these results to centers lacking similar laparoscopic biliary expertise. We suggest that broader adoption of single-stage LCBDE should be accompanied by structured training programs and resource investment in laparoscopic biliary techniques to ensure safe implementation and reproducible outcomes across different care settings.
Limitations
This study was performed at a single tertiary referral center and thus may be subject to center-specific practice patterns and resource availability, which limits generalizability. Operator-dependent variability in technique and experience may have influenced outcomes despite comparable surgeon caseloads. Cost estimates reflect institutional charges and may not directly extrapolate to different health systems. Finally, a post-hoc power analysis indicated that although the sample size provided adequate power for the primary endpoints (length of stay, pain), the study had limited statistical power (~65%) to detect small differences in rare adverse events, and thus, subtle safety differences between the two approaches cannot be excluded.
Future multicenter trials should be powered specifically to detect clinically meaningful differences in rare but important adverse events; for example, detecting a 2% absolute difference in major complications with 80% power would require a substantially larger sample size than the present study.
Conclusions
Single-stage LCBDE provides a safe, efficient, and cost-effective alternative to ERCP+LC, offering comparable duct clearance, lower early postoperative pain, and a trend toward shorter hospitalization. Although the univariate difference in length of stay did not reach statistical significance, multivariate analysis identified ERCP as an independent predictor of prolonged stay; combined with the clear resource advantages (single vs two procedures, lower aggregate OR time and costs), these findings support adoption of LCBDE in experienced centers while simultaneously advocating for structured training programs as a prerequisite for broader, safe implementation. For patients with unfavorable anatomy, very high operative risk, or when endoscopic expertise predominates, the staged ERCP approach remains an important alternative. Larger multicenter and randomized studies with extended health-economic and quality-of-life endpoints are warranted to confirm these findings and to refine selection algorithms.
Acknowledgment
The authors would like to express their sincere gratitude to the Department of General Surgery, Faculty of Medicine, Sohag University, for continuous support and cooperation during the study.
Special thanks are also extended to the operating room nursing staff and residents for their assistance in patient care and data collection.