Introduction
A lot of things have changed in our way of living and learning because of the rapid development of technology. According to Tang et al. (2022),1 the educational sector has adopted technology and Virtual Reality as one of these tools. Virtual reality is an interactive technology that allows individuals to engage in real-time with a virtual environment, allowing them to play, explore, reflect, and make errors without having any consequences in the actual world. There are, according to Bacca et al.,2 several advantages of using virtual reality in the classroom, including addressing concerns about patient safety, lack of cadavers and other constraints on resources. Furthermore, Gunn et al.3 demonstrated that the use of virtual reality can be an incentive and effective way to increase user confidence and knowledge as well as skills development.
Virtual reality is also a great way for students to practice and repeat complicated tasks such as surgical training. In addition, Dhar et al.4 stated that when remote learning became a necessary part of the COVID-19 epidemic and demand for electronic resources and simulations increased significantly, the development of virtual reality was more important than ever before.
In several studies, virtual reality was evaluated as useful for therapeutic skills training, and the results were positive. For example, a meta-analysis of 15 studies on the use of virtual reality in healthcare training by Zhao et al.5 found that VR-based education was associated with significant impacts on learning outcomes such as information retention, test scores, and learner satisfaction. In a second study carried out by Vrillon et al.,6 it has been found that VR Training is more effective than traditional training methods on the lumbar puncture in enhancing performance and skill acquisition among medical students.
The potential of virtual reality simulators to provide learners with rapid feedback is another advantage that Gan et al.7 examined. In addition, it can be performed in real-time so that users have a chance to think about their actions and make more accurate decisions. This shifts the learning pathway from passive to active, which is beneficial for long-term retention.8
Despite the use of VR in healthcare training for many years, there is still a lack of data on how it will be used over time. In addition, the widespread use of virtual reality in education is hampered by the high cost of the application of VR in education.7 However, as scientific and technological progress takes place, those costs will probably decline over time leading to greater accessibility for institutions and students.
It is essential to analyze the usefulness of VR in increasing the skill level of students studying medicine at university degree level, given its potential for improving healthcare skills and patient outcomes.
Methods
There were 8 participants, third-year undergraduate medical students from Trinity College Dublin (TCD), Ireland. The students had 4 months of experience on clinical placements at the time of this study and were in the 18-25 age range. Ethical approval was granted by the School of Medicine, TCD Ethics Committee and all participants provided consent.
The study consisted of 2 phases. The first phase involved an orientation session in which participants spent 10-15 minutes on an orientation session with the VR headset. This helped to familiarize the participants with the VR technology and how to use it.
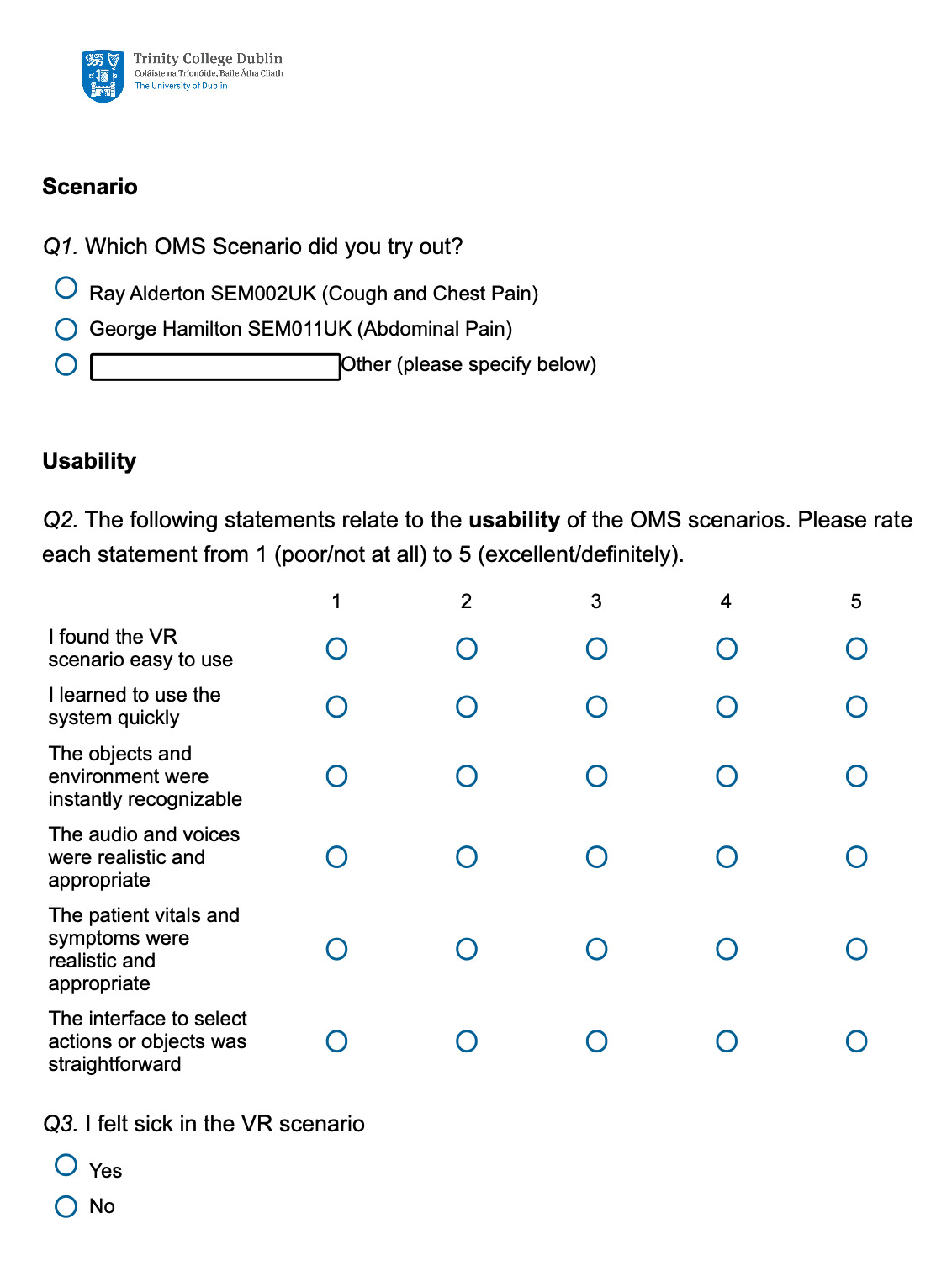
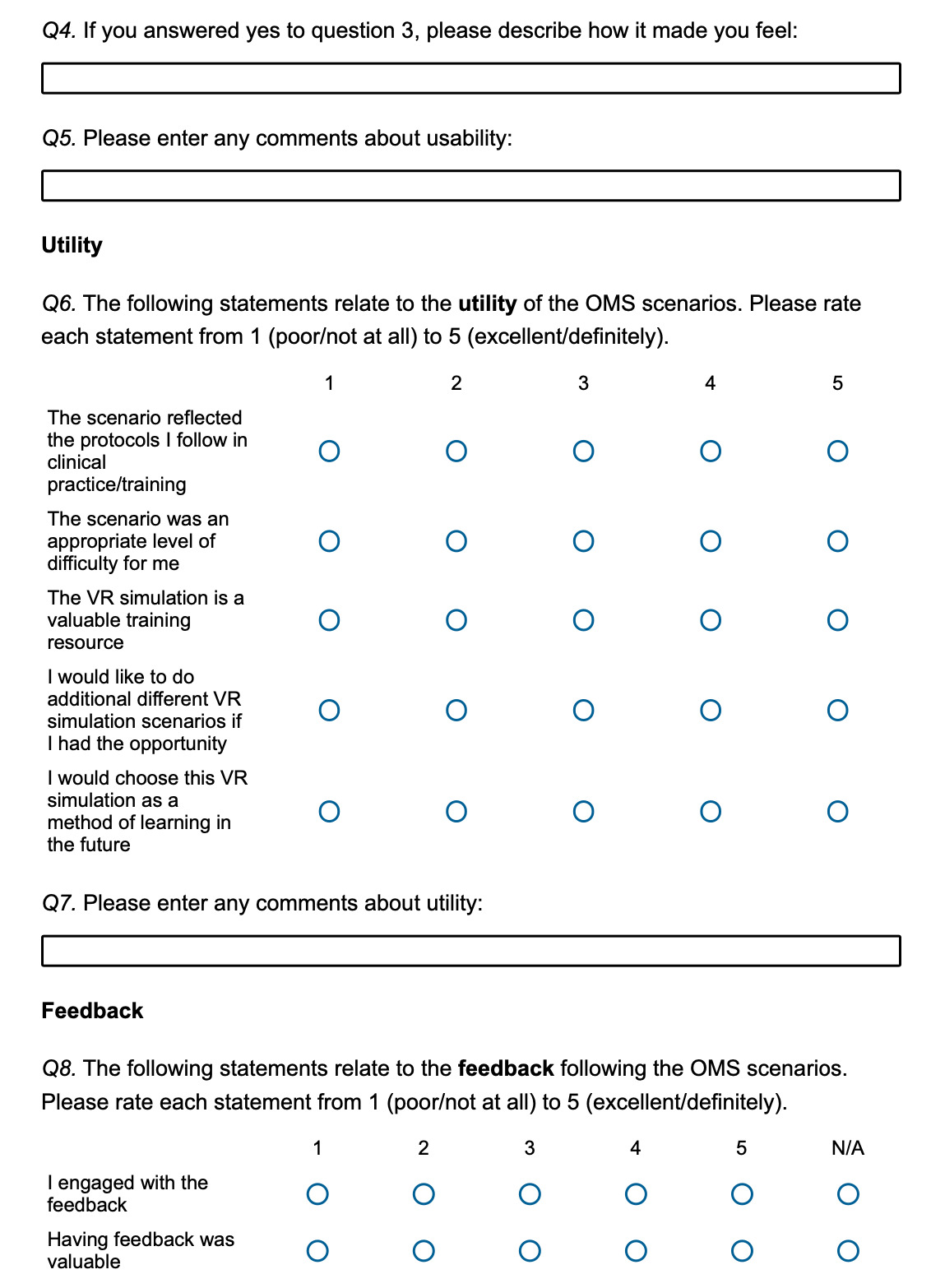
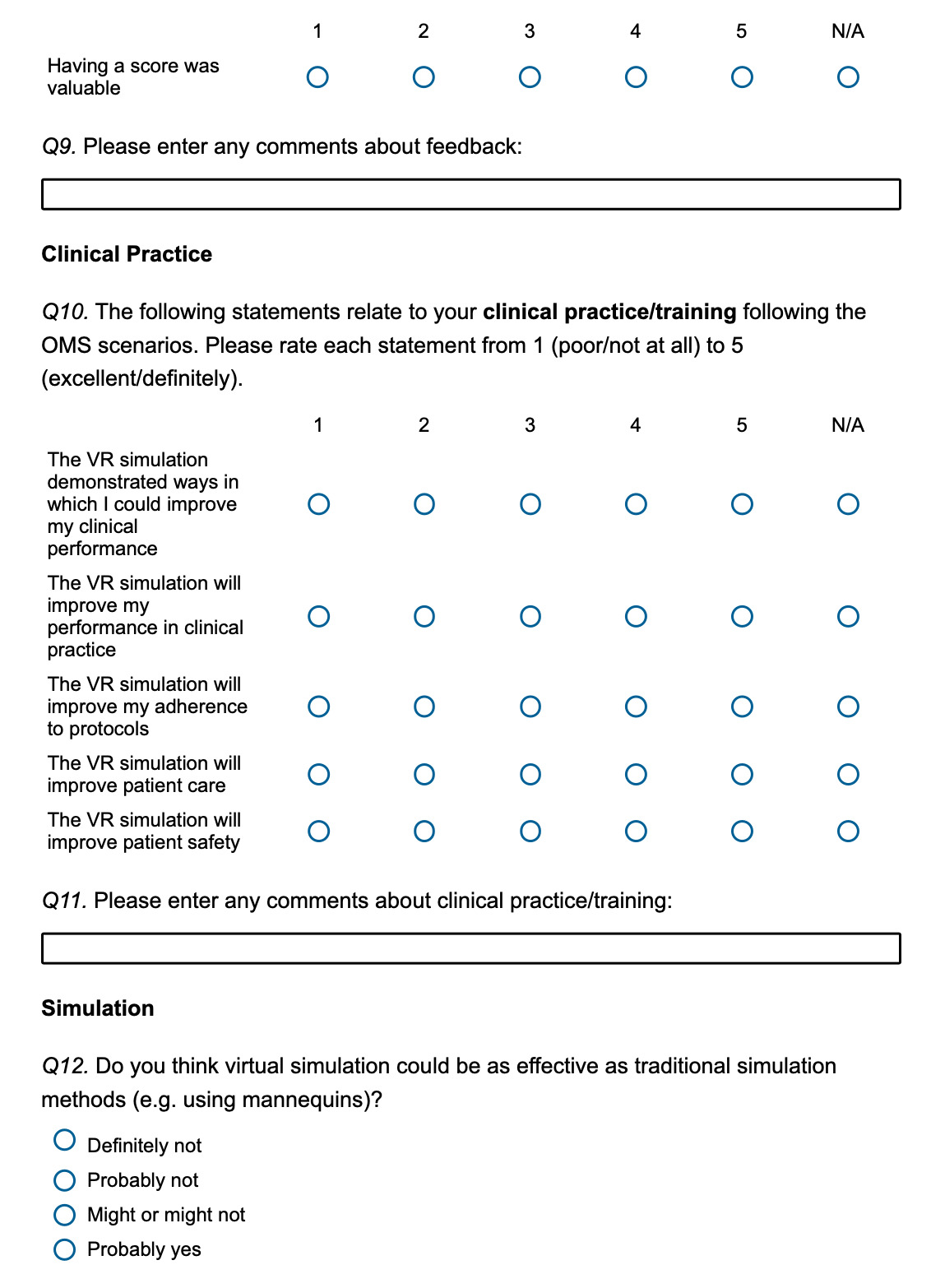
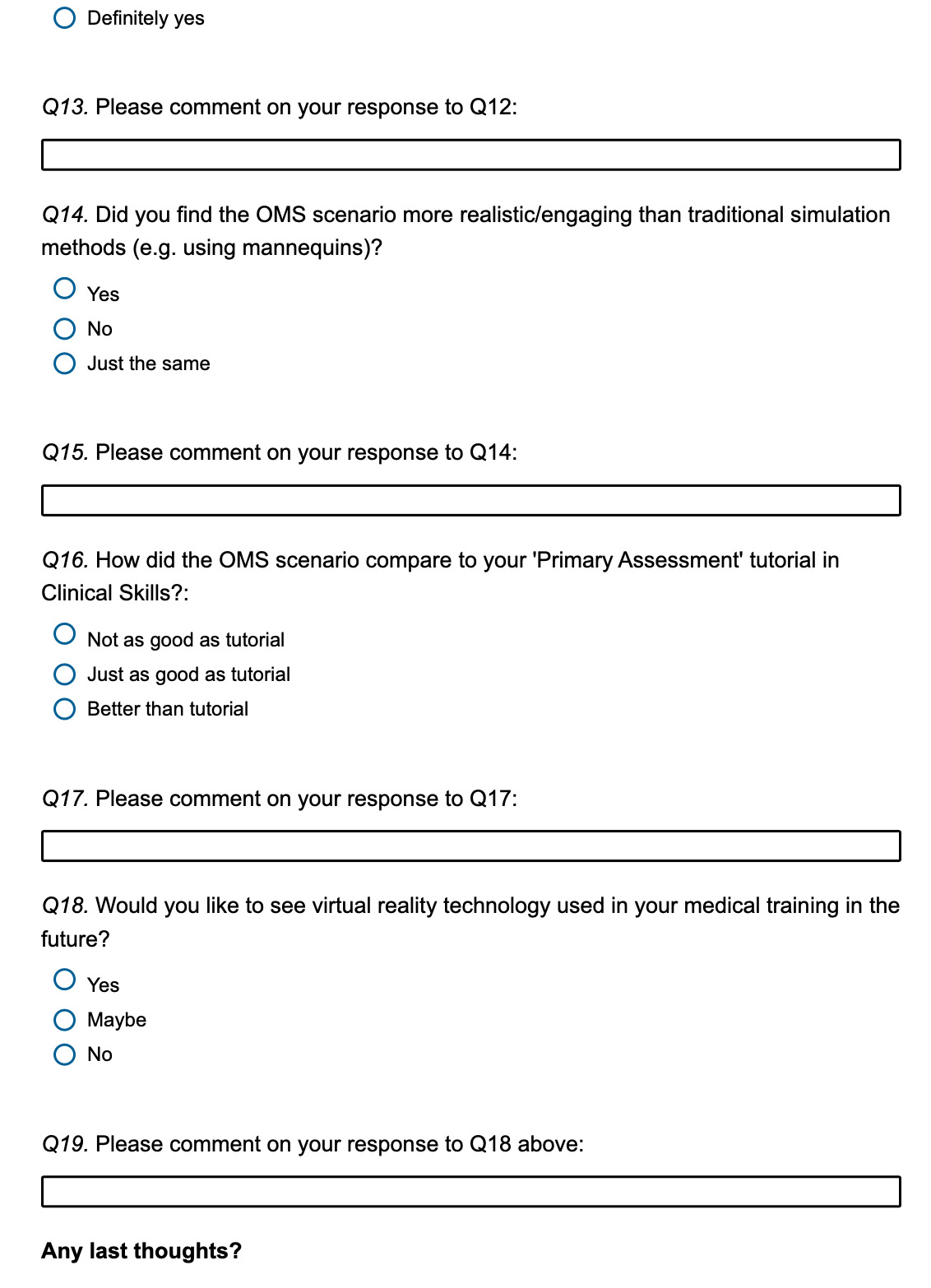
The second phase involved participants engaging in a VR emergency clinical scenario (anaphylactic reaction, abdominal pain or sepsis), images 1 and 2. The software allows participants to simulate the treatment of a wide range of conditions.9 Each scenario has a time limit of approximately 15 minutes and participants were given a comprehensive feedback review by the software. Following this session, participants were asked to complete a Qualtrics® questionnaire anonymously to evaluate their experience. The questionnaire contained 20 questions most using a 5-point Likert scale (Appendix 1). The questionnaire focused on how participants felt about the usability, utility and feedback as well as the relevance to clinical practice.
Results
Participants (n=8) completed a questionnaire on the usability, utility and feedback following their clinical emergency scenario. The questionnaire also asked participants to compare the use of VR to the equivalent traditional teaching method using a SimMan® 3G high fidelity mannequin. Responses to the questionnaire were recorded on a 5-point Likert scale.
Realism
Participants consistently scored the software very highly in all aspects of realism, the questions asked if “The objects and environment were easily recognizable” (mean of 4.75 and standard deviation of 0.4), “The audio and voices were realistic and appropriate” (mean of 4.75 and SD of 0.4), “The patients’ vitals and symptoms were realistic and appropriate” (mean of 4.75 and SD of 0.4).
Interface and Usability
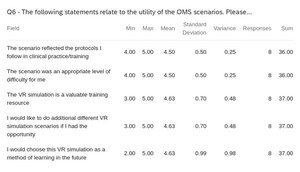
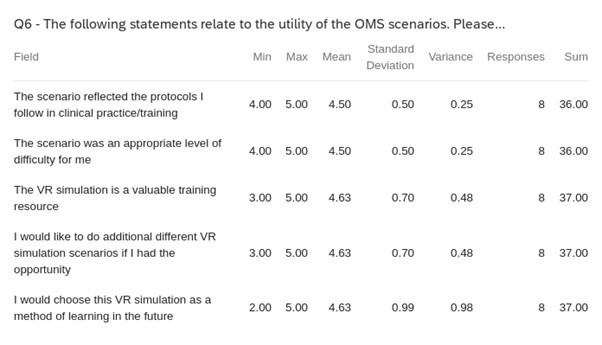
The ease of use and overall impressions of the software are given in Table 1. Participants found the VR scenario easy to use (mean of 4.38 and standard deviation of 0.7) but found the interface to be not exceptionally straightforward, results to the prompt “The interface to select actions or objects was straightforward” were variable (mean of 4 and standard deviation of 1.12), But the participants learned to use the interface quickly, mean of results to the prompt “I learned to use the system quickly” was 4.75 with a standard deviation of 0.43).
None of the participants felt sick during the VR session. Overall, the participants uniformly scored the software highly in realism and thought that the VR scenario was easy to learn and use, with varying results on the difficulty to select objects or actions.
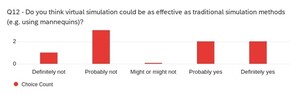
Utility of the scenarios
The use of the software as a learning tool for the participants can be seen in Table 2. Participants scored the software very highly in Utility with a low standard deviation across all questions. Participants thought strongly that the VR scenario reflected the protocols used in clinical practice, (mean score of 4.50 SD of 0.5). The level of difficulty of the scenario was deemed appropriate with a mean of 4.5, SD of 0.5 in response to “The scenario was an appropriate level of difficulty for me.” Participants thought that VR simulation is a valuable training resource (mean of 4.63 and SD of 0.70).
This software received good feedback and participants showed very strong enthusiasm to try other VR scenarios, “I would choose this VR simulation as a method of learning in the future” (mean of 4.63 and SD of 0.99), “I would like to do additional different VR simulation scenarios if I had the opportunity” (mean of 4.63 and SD of 0.7).
Overall, regarding Utility, participants strongly agreed that this VR software is worthwhile and a good and suitable training resource and showed enthusiasm to attempt more scenarios.
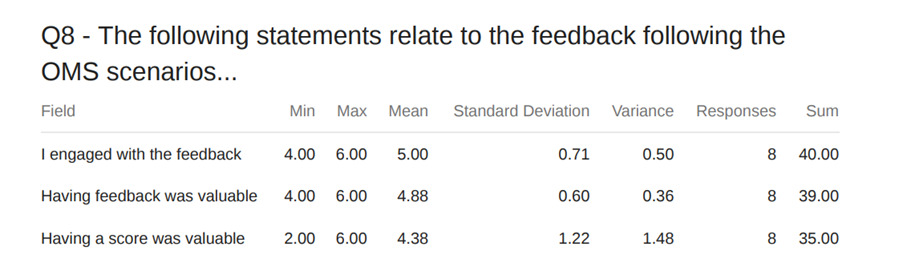
Feedback following the scenarios
The software provides feedback at the end of each session; participants were asked about this feedback (Table 3).
Participants who engaged with the feedback felt that it was very useful, (a mean score of 5 and SD 0.71). However, there were variable results regarding the overall scenario percentage score given as feedback at the end of the scenario. Responses to “Having feedback was valuable” had a mean score of 4.25 and a standard deviation of 1.30 and responses to “Having a score was valuable” had a mean score of 4.38 and 1.22.
One participant commented, “I think the idea of automatic, personalized feedback and grading is one of the strongest arguments for VR scenarios in medical training.” “Feedback is really in-depth, more than a human could provide.” Overall participants agreed that the feedback was valuable with some mixed but overall positive regarding the percentage score received at the end of the VR scenario.
Clinical Practice and Training
Participants were asked a set of questions to determine if VR simulation could aid in their Clinical practice/training. Participants largely agreed that the VR simulation demonstrated ways in which they could improve in clinical practice and training, (mean score of 4.625 and SD of 0.48). The responses to the prompt “The VR simulation will improve my performance in clinical practice” received a mean score of 4.125 however there were a couple of outlier scores of 2 which resulted in a standard deviation of 1.17. The results were similarly varied on “The VR simulation will improve my adherence to protocols” mean score of 3.88 and a standard deviation of 1.36 with an outlier 1 score. One participant commented “one scenario wouldn’t be enough to make an impact on learning and adherence- but with multiple and consistent usage it would do all of the above (5/5).”
Patient safety and care
Participants generally agreed with the prompt “The VR simulation will improve patient care” with one outlier score of 2 (mean score of 4.125 and standard deviation of 1.05) and similar results with “The VR simulation will improve patient safety” (mean score of 3.875 and standard deviation of 1.45) outlier scores of 1 and 2. The results for this section were varied with high standard deviations due to some outliers.
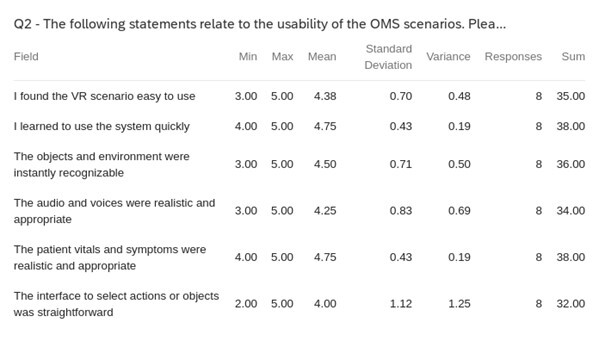
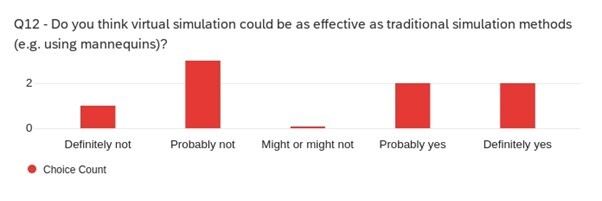
The participants were then asked a set of questions comparing VR simulation with traditional simulation used in clinical training. The responses to the question “Do you think virtual simulation could be as effective as traditional simulation methods (e.g., using mannequins)?” were varied (Fig. 1). Participants commented “As someone who has had extensive medical manikin training (due to Sim wars), I don’t think VR can fully replace it. Learning how to use the emergency trolley, learning where to find things (rather than having pre-set options and questions), how to place cannulas, where to listen on the chest/lungs, taking a pulse, learning how the equipment looks like and how to adjust it (e.g. Venturi masks/non-rebreathers), just to name a few things, are skills that must be done physically, and with mannequins being the closest thing to a patient, I think they will still remain a valuable learning source.”
“VR is not a replacement for conventional clinical scenario training, such as a practical clinical procedure or communication with colleagues or communicating with patients. it does however allow a memorable and useful way of practicing theory and algorithms we have learned in lectures. I don’t think VR replaces any teaching; it should be viewed as its own additional tool for learning.”
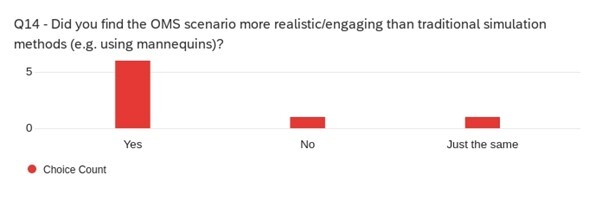
The participants found the scenario to be more realistic than traditional methods, “Did you find the scenario more realistic/engaging than traditional simulation methods (e.g., using mannequins)?” (Fig. 2) with comments such as “They are engaging in different ways! Since mannequin training is done without any hints, it is slightly more challenging (you must come up with your own questions, remember how to take a history, remember drugs and doses, remember appropriate blood tests without any prompt!).” “They aren’t comparable!! Sure yes, the VR would be better than one-on-one training with a mannequin, but the mannequin allows for a lot of flexibility but requires more expensive equipment and someone to run the mannequin. The VR is standalone and could be done by yourself.”
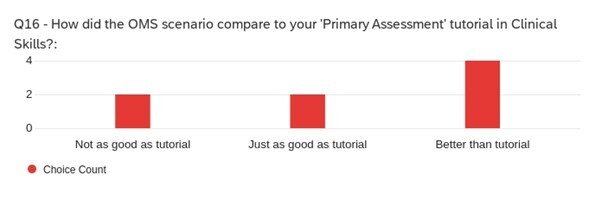
Participants were asked to compare the VR scenario training to a ‘Primary Assessment’ tutorial they had recently participated in which uses a SimMan® 3G high fidelity mannequin. The responses to the question “How did the scenario compare to your ‘Primary Assessment’ tutorial in Clinical Skills?” were mixed (Fig. 3). Some comments made by participants were, “Tutorial was good but stunted by the mannequin not being responsive.” “Showed the bigger picture.”
Overall participants think VR is a useful tool in medical training, that has some strong advantages over traditional training and agreed that they were interested in VR technology being used for medical training in the future.
Discussion
The software appears to have immense potential to be incorporated into the medical curriculum. It is a source of untapped potential, providing realistic scenarios and comprehensive post-scenario feedback reviews. Overall, the participants shared the view that this VR software was detailed and helpful in providing a full breakdown of the participants’ scores and providing a comprehensive review of the entire scenario should they fail to achieve a complete diagnosis. However, one participant noted that this VR technology was beneficial to the reinforcement of knowledge learned during lectures but should not be seen as a replacement for other forms of Clinical Skills teaching methods. Instead, it should be seen as its own additional learning tool. The main reason for their response was that during the scenario, the physical examinations section was brief and did not demonstrate fully how each type of physical examination was conducted. Another participant also mentioned the time constraints present during the software use. The approximate time limit of 15 minutes led to participants feeling rushed to complete it although this may have been due to inexperience.
The participants had a largely positive experience with the VR headset and software. They considered it to be an engaging experience, especially for those who have never tried VR before and could be incorporated into the medical curriculum as a valuable learning tool.
Limitations
The sample size was limited to 8 volunteer students who may have had a particular interest in using VR for clinical skills training. Hence, the results might not apply to a wider population of students. Future research should try to include larger numbers and more diverse students to enhance the validity of the findings. The participants completed only one or two scenarios and had they completed more scenarios would have had a wider breath of experience to address the potential benefits and drawbacks of VR use in medical training. Therefore, a future improvement to the study would be to allow participants to interact with the VR headsets for longer periods and complete more scenarios.
Conclusion
In conclusion, adding VR to Clinical Skills training has many benefits. VR is a technology that is constantly improving, and the disadvantages may be addressed in future developments. This technology may not be ready to fully replace the traditional face-to-face methods of learning Clinical Skills, but they can serve as an additional learning tool for students to reinforce their knowledge. As VR improves and its hardware becomes more accessible, more will start to consider its incorporation into the medical field, be it in medical school or in teaching hospitals across the world. This study gave a glimpse into the expansive world of VR and how it can be weaved into the fabric of medical education in the years to come, revolutionizing the way student doctors learn and practice medicine.
Abbreviations
OMS Oxford Medical Simulation
VR Virtual Reality
SD Standard Deviation
Declaration
We declare no conflict of interest.
Author’s Contributions
All authors were major contributors in writing the manuscript, either participating in the survey development, data analysis, writing of the paper, or the editing process. The authors read and approved the final manuscript.