Introduction
Ischemic stroke, also known as cerebral infarct, is when blood vessels leading to the brain are blocked, preventing oxygen and other nutrients in the blood from reaching the brain and its cerebral tissue. About 87% of all strokes are ischemic strokes.1 People who have increased risks of strokes in general include people of older age, especially those who are 65+ years, females, and those of the African American race. Risk factors specific to ischemic stroke include smoking, hypertension, hypercholesterolemia, and diabetes mellitus (DM).2
An acute left parietal infarct results from the sudden occlusion of blood flow to the left parietal lobe. The lack of blood in the left parietal lobe results in increasing damage to the tissues and neurons over time. This damage often presents as right-sided weakness, and/or difficulty performing motor tasks on the right hemisphere of the body.3 It may also present as language issues, such as slurred speech or stuttering.4,5 Some infarcts in the left parietal lobe can result in a disorder called Gerstmann Syndrome, which presents as difficulty in writing (agraphia), difficulty calculating basic math (acalculia), difficulty in identifying fingers (finger agnosia), and left-right disorientation.6,7 [Figure 1]. This was the case with our patient. Others may be associated with right-sided Alien Hand Syndrome (AHS), in which patients develop an estrangement from, and loss of motor control of a limb located on the right hemisphere of the patient’s body.8–10 Early detection of these symptoms leads to an early diagnosis and prompt treatment of stroke.
Case Presentation
The patient is a 66-year-old African American male who presented with right-sided arm and leg weakness, as well as slurred speech. In addition, he showcased all four symptoms of Gerstmann Syndrome. Symptoms were observed around 5 am after the patient woke up. He was then evaluated in the Emergency Department (ED) at 8:40 am. A stroke alert was called during the evaluation at 8:38 am.
During the evaluation, vital signs included a temperature of 98.5°F, blood pressure (BP) of 180/110 mmHg, heart rate (HR) of 82 breaths per minute, respiratory rate (RR) of 20 breaths per minute, and a pulse oximeter of 93% on room air. The patient had a past medical history of hypertension and diabetes, as well as a habit of smoking a pack of cigarettes per day for the past 40 years. On arrival, a neurologic examination revealed a National Institutes of Health Stroke Scale (NIHSS) score of 5, with one point each for each for items 1b, 5a, 5b, 9 and 10.
During the patient’s time in the ED, a Computed Tomography (CT) Scan of the head was taken at 8:48 and did not reveal any evidence of hemorrhage. A Computed Tomography Angiography (CTA) Scan of the head and neck did not reveal the presence of a large vessel occlusion (LVO).
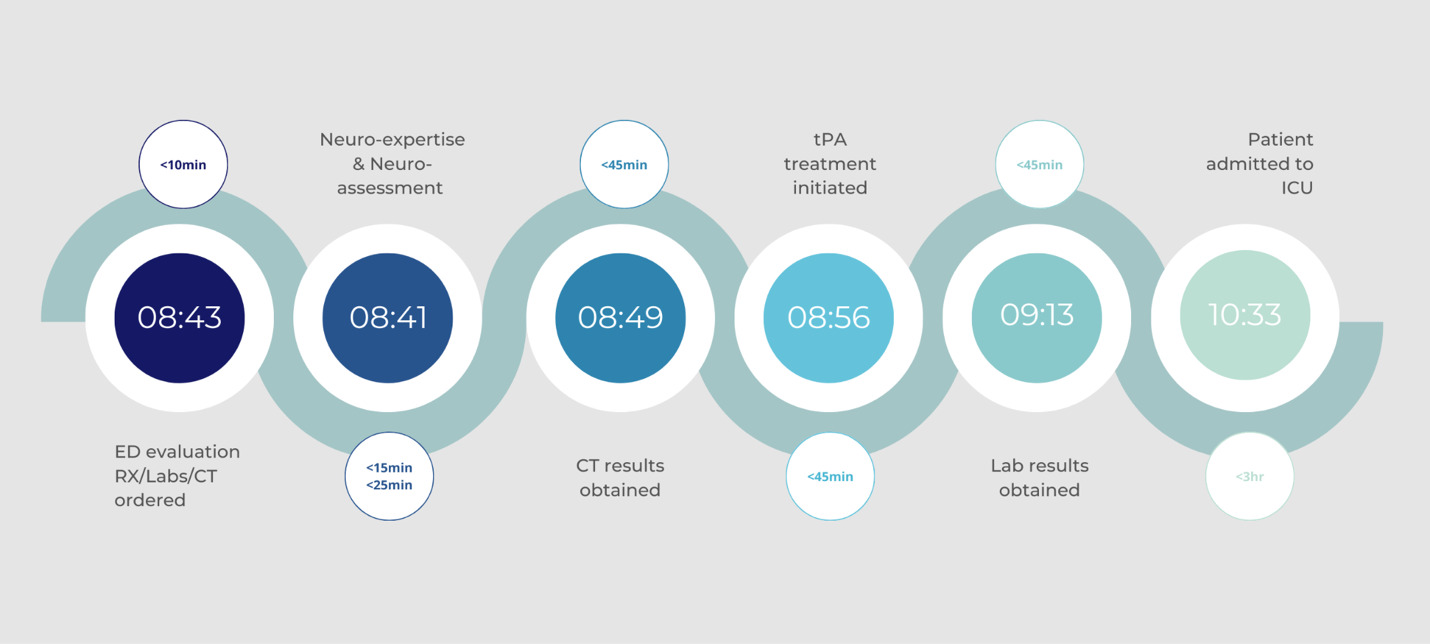
Inclusion and exclusion criteria were reviewed, and the patient met the criteria for Tissue Plasminogen Activator (tPA) administration. Medication was initiated in the ED at 8:56 am, and the patient was later admitted to the Intensive Care Unit (ICU) at 10:33 am [Figure 2].
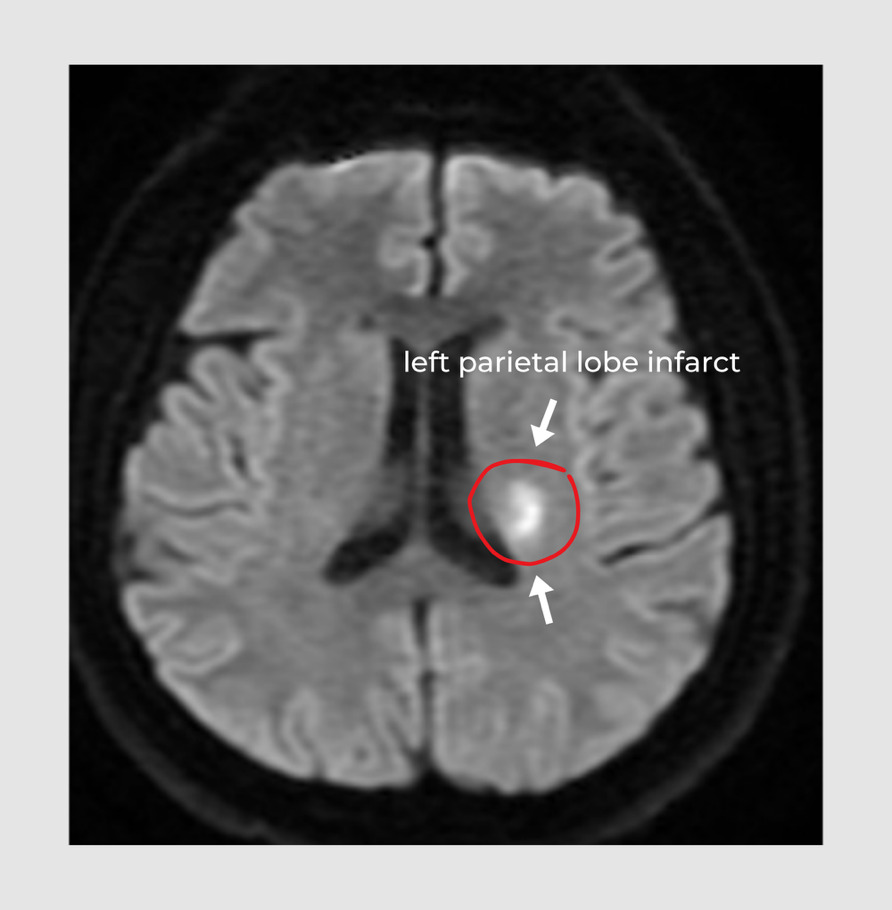
Subsequent magnetic resonance imaging (MRI) of the brain showed acute infarction of the left parietal lobe, displayed by the small white area [Figure 3].
On the second day in the ICU, the patient’s symptoms improved, and his NIHSS decreased to three. The patient had a Transesophageal Echocardiogram (TEE) done, which was reported as normal, excluding cardioembolic events and patent foramen ovale. His blood work, including cholesterol, thyroid, comprehensive metabolic panel (CMP), complete blood count (CBC), and international normalized ratio (INR) were normal.
Discussion
The patient had an increased risk of stroke because of older age (66 years old) and race (African American), and acute ischemic stroke because of his smoking habits, history of hypertension, and diabetes.1 African Americans are 3.9% more likely to experience a stroke in their lifetime compared to their White, Hispanic, and Asian counterparts.11 Their increased rate of strokes is mainly due to a higher prevalence of risk factors associated with stroke, including diabetes and hypertension.12–14 In addition, this specific demographic has a greater likelihood of developing Sickle Cell Disease (SCD), which can increase the overall risk of both ischemic and hemorrhagic strokes.15
The patient showed symptoms of right-sided arm and leg weakness and slurred speech. Additionally, he presented all four symptoms of Gerstmann Syndrome including agraphia, acalculia, finger agnosia, and left-right disorientation. Gerstmann Syndrome typically occurs when there is a lesion in the left parietal lobe (angular gyrus), and rarely in the right parietal.6,7 It was confirmed he had a left parietal infarct shown by a small white spot in the MRI scan. Although he had an infarct, he did not show any symptoms of Alien Hand Syndrome. Some factors that could be considered regarding the wide range of symptoms for a left parietal lobe infarct include the vast different structures (tissues, cells, neurons, etc.) corresponding with different functions that are damaged, the length of time since the left parietal lobe has been cut off from blood supply, and the size or extremity of the area affected.
The patient’s oxygen saturation (93%) was slightly lower than the recommended average (94%-100%) and may contribute to loss of consciousness and/or impairment of reflexes in other similar cases. These consequences of low oxygen saturation may risk interfering with the testing process for stroke. Failure to improve the pulse oximetry may also result in secondary injury to the brain.16 Another abnormal vital sign observed is high blood pressure (180/110 mmHg), indicating hypertension. In addition, the patient already had a past medical history of hypertension. Patients with severe hypertension are at risk of hemorrhagic transformation (HT), and the risk is further increased if patients are administered IV-tPA. Therefore, blood pressure should be closely monitored; BP should not exceed 185/110 mmHg prior to IV-tPA administration and should be lowered to below 180/105 mmHg once IV-tPA has been given.16 In this case, the patient had a blood pressure of 180/110 mmHg during his initial ER evaluation and qualified for tPA, which was administered 16 minutes later. As the patient had a normal TEE reading on the second day, it can be inferred that his blood pressure was adequately monitored and lowered to a normal range.
The patient’s CHA2DS2-VASc score adds up to three— one point each for being between 65-74 years of age, having a history of hypertension, and having a history of DM. His score of three indicates that he had a 3.2% risk of stroke. Patients with a CHA2DS2-VASc score of two or higher are classified as high-risk and are treated with oral anticoagulants (OACs).17,18
Conclusion
Left parietal lobe infarcts have a variety of symptoms, ranging from motor difficulty on the right hemisphere of the body to language deficits, to disorders like Gerstmann Syndrome. The vast range of symptoms associated with acute left parietal infarcts makes awareness and understanding of these indications crucial to efficiently diagnosing and treating them accordingly.
Statement of Ethics
This retrospective review of patient data did not require IRB or other ethical approval in accordance with local/national guidelines. Written informed consent was obtained from the individual for publication of the details of their medical case and any accompanying images.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
This study was not supported by any sponsor or funder.