Introduction
The widely used method of contraception worldwide is the intrauterine contraceptive device (IUCD), offering reversible long-acting contraception benefits to its users. They are 99 per cent effective in preventing pregnancies. However, some of their rare complications are usually overlooked. Uterine perforation is seen in 0.3 to 2 per 1000 insertions of IUDs and may often land the patient in severe circumstances, including intestinal obstruction and perforations, which are usually life-threatening.1
With an increasing use of IUDs over the past decades, the risk of this rare complication is on the rise. Here, we present a case of an asymptomatic young lady with an obstetric score of G3P2L2 who was planned for medical termination of pregnancy (due to unexplained contraceptive failure).
Clinical Description
A 23-year-old woman presented for medical termination of her third pregnancy. She used an intrauterine contraceptive device (IUCD) inserted a year ago. Her last period was nine weeks ago. She had no abdominal pain or bleeding.
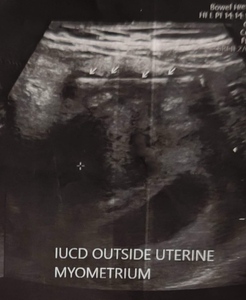
Examination revealed stable vitals, a soft, non-tender abdomen, and a normal vaginal exam. Ultrasound revealed an 8-week singleton pregnancy, with the IUCD abutting the anterior uterine wall, sigmoid adhesions, and omental wrapping. [Fig 1]
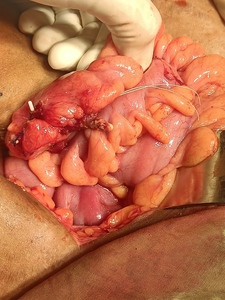
She was scheduled for an exploratory laparotomy after pregnancy termination. A Pfannenstiel incision was made for tubectomy and IUCD removal. The fallopian tubes were visualised, and modified Pomeroy’s tubectomy was done. During surgery, the anterior uterine wall was perforated, with the IUCD embedded in bowel loops (sigmoid colon and ileum) with omental wrapping. [Fig 2]
Dense adhesions between the mesocolon and uterus were found. Surgeons released these adhesions, revealing sigmoid colon perforation by the IUCD. The IUCD was removed, the bowel perforation repaired with sutures, and hemostasis achieved. [Fig 3] The abdomen was closed with a pelvic drain. Postoperative recovery was uneventful, and she was discharged on day 8 after drain removal.
Discussion
Intrauterine contraceptive devices (IUCDs) are the most effective form of contraception, with the rates of failure almost similar to various forms of sterilisation, effective in preventing 99% of pregnancies. They are the preferred mode of contraception owing to their ease of use and reversibility.2
All IUCDs are T-shaped, 28-30mm in width and 30-36mm in length, with the top of the T designed to rest on the top of the endometrial cavity. The smallest IUCDs are preferred for nulliparous young women.3 They are indicated for the use of contraception and are approved for 5 years.4
Uterine perforation is a serious complication of IUCD insertion, which can be an immediate or a delayed event. The incidence of IUCD perforation is 0.87 per 1000 insertions,5 And is associated with various factors like the time of IUCD insertion, IUCD type, skills of the attending physician, and anatomy of the uterus. The contributing factor for migration involves the inadequate assessment of the size and position of the uterus with an IUCD. Ultrasound is the first-line investigation for the assessment of IUCD migration and helps in the determination of the position. In suspected cases of extrauterine migration, a radiograph of the abdomen with magnetic resonance imaging is required.6
Management of the migrated IUCDs is controversial. The World Health Organisation advocates the removal of all migrated IUCDs, irrespective of type and location.7 The crucial reason for this strict recommendation is the damage and complications like closed-loop obstruction, actinomycosis, and intestinal perforation that result if left in situ.8 16 cases described by Heinonen et al. depicted the need for laparotomy in migrated IUCD adherent to omentum or sigmoid colon.
A systematic review conducted by Victoria Verstraeten et al. in 20249 Included 119 cases. The average age of patients was 39 years, and 46% of cases complained of abdominal pain as the most common symptom. However, about 31 per cent of patients were asymptomatic. The time interval between IUCD placement and diagnosis ranged from 1 week to 42 weeks, with a median of 3.75 years. The most common location of a displaced IUCD is the intestines (rectum -12%), but here, we have an IUCD that was embedded in the sigmoid colon.
Conclusion
The intrauterine contraceptive device (IUCD) is the most commonly used form of contraception among females. It provides numerous advantages, such as being reversible and easy to use. Additionally, it’s crucial to recognise and be aware that the use of such devices can sometimes lead to serious and long-term complications, demanding a major surgical intervention.
Ethical Considerations
Informed consent was obtained from the patient for publication of this case report.