Case Presentation
A 76-year-old woman presented to the emergency department with acute-onset abdominal pain, low back pain, and generalized weakness for one day. She had a past medical history significant for stage III chronic kidney disease, left renal cell carcinoma treated with nephrectomy without chemotherapy in 2023, deep vein thrombosis (DVT), gastroesophageal reflux disease (GERD), and bladder cancer. She was presenting status post robotic hysterectomy for spread of bladder malignancy to the uterus and bladder reconstruction surgery, performed three days prior.
On physical examination, she was hypotensive (97/53 mmHg), tachycardic (128 beats per minute), and afebrile (97.5 degrees Fahrenheit). Her respiratory rate was 18 breaths per minute, and oxygen (O2) saturation was 95%. Her abdomen had generalized tenderness, and guarding was present. There was a region of large purple ecchymosis extending from the umbilicus to the left lower abdominal quadrant and left flank (Figure 1).
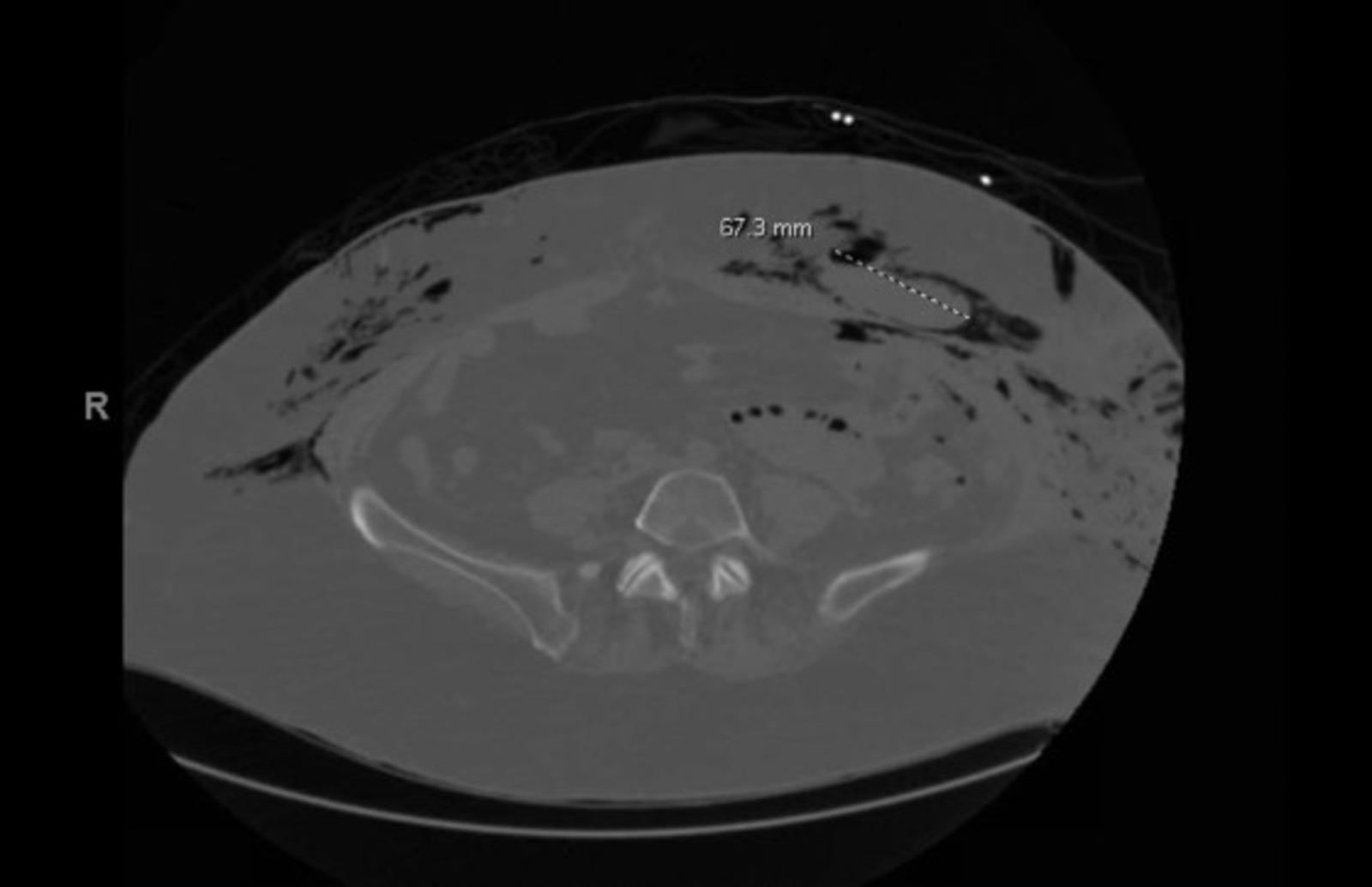
During the first day of her hospitalization, the patient underwent a computed tomography (CT) scan of the abdomen and pelvis which revealed a large pneumoperitoneum; soft tissue density in the anterior abdominal wall measuring 7.5 cm on the left, which may represent a hematoma; a stomach distended with fluid as well as fluid-filled loops of small bowel without definite transition zone, indicative of ileus; and gas within the small bowel wall, suggestive of bowel infection or trauma. The extensive subcutaneous and intramuscular air involving the abdominal wall extending up into the chest on CT raised concern for necrotizing fasciitis (Figure 2).
The patient’s laboratory findings were significant for leukocytosis, lactic acidosis, anemia, thrombocytopenia, elevated creatinine, and increased International Normalized Ratio (INR) (Table 1).
Blood cultures were also obtained on her first day of hospitalization and did not reveal any organisms. The patient was initially treated with piperacillin-tazobactam and vancomycin for broad-spectrum coverage of the intra-abdominal source of infection, but she continued to deteriorate throughout the course of her hospital stay. She was managed with IV fluids, continuous antibiotic treatment, and vasopressors for persistent hypotension.
The patient was scheduled for a diagnostic laparoscopy with open laparotomy for the abdomen and pelvis on day 2 of her hospitalization. At the time of laparoscopy, the patient had bilious staining in the left lower to mid-abdomen. Open exploration of the abdominal wall in the left lateral aspect revealed evidence of small bowel succus in the subcutaneous tissues with infection and necrosis, suggestive of inadvertent bowel injury from the prior surgery and development of necrotizing infection. All necrotic and infected tissue was debrided, and irrigation was performed with chlorhexidine gluconate and saline (Irrisept). She was then admitted to the medical intensive care unit (MICU) and continued on vasopressors and antibiotics.
The patient returned to the operating room (OR) the next day where progressive necrotizing fasciitis was found involving the left lateral abdominal wall and extending to the anterolateral left thigh. Three additional surgical debridement procedures were performed over the next five days. The patient’s necrotic tissue progressively decreased over time, eventually requiring no further debridement. The patient was placed on two wound vacuum-assisted closures (VACs) to facilitate healing. The patient was discharged with IV ceftriaxone 2 g daily and oral metronidazole 500 mg TID to complete a two-week course due to the severity of the patient’s infection, and she was followed up with general surgery and wound care specialists for future debridements, change of dressings, and wound VAC management.
Discussion
Necrotizing fasciitis (NF) is a severe, life-threatening soft tissue infection that involves the necrosis of tissues and fascial planes. Most commonly caused by group A Streptococcus (GAS), necrotizing fasciitis spreads quickly through the fascial plane and beyond, with the body responding with an intense inflammatory reaction. However, this inflammatory response is often inadequate due to the rapid spread of infection, leading to systemic infection, sepsis, and multiorgan failure.2 Our case of a 76-year-old female patient who developed necrotizing fasciitis just three days after abdominal surgery highlights the rapid and aggressive nature of the infection and emphasizes the importance of early detection and immediate surgical intervention. For our patient, the initial surgical exploration on the second day of hospital stay was crucial in the diagnosis and timely removal of necrotic tissue. The small bowel injury revealed on CT imaging and subsequent surgical exploration – likely an inadvertent injury from her recent abdominal surgery (i.e., hysterectomy, bladder reconstruction surgery) – served as a probable source of our patient’s necrotizing infection.
Surgery involving the abdomen is a well-known risk factor for necrotizing fasciitis, with many cases in literature demonstrating this association. One example is the 58-year-old woman presented by Fozo et al., who developed necrotizing fasciitis of the anterior abdominal wall three weeks after undergoing laparoscopic sleeve gastrectomy with hiatal hernia repair.3 Another instance is the 46-year-old woman discussed by Pantelić et al., who developed NF on the eighth postoperative day after her total abdominal hysterectomy. Necrotizing infection of the skin and subcutaneous tissue developed around the incision site, and she would not be discharged until day 19 of hospitalization.4 Makhdoomi et al. presented a 27-year-old woman with necrotizing fasciitis involving the lower anterior abdominal wall ten days after a lower segment Cesarean section.5
Similar to our case, immediate surgical intervention and aggressive debridement led to the complete recovery of all three patients. However, one significant distinguishment between our patient and the reports in literature of abdominal surgery-related NF is the rapidity of disease progression. While many of these cases involve patients developing necrotizing soft tissue and subcutaneous infection multiple days to weeks after abdominal surgery, our patient developed NF within three days of her robotic hysterectomy and bladder reconstruction surgery, highlighting the unique nature and severity of our case.
The challenge in diagnosing necrotizing fasciitis is often complicated by the presentation of vague symptoms at initial onset. In this case, our patient presented with vague symptoms of abdominal pain, low back pain, and weakness. Due to the wide array of conditions that present with these same symptoms (e.g., aortic aneurysm, spinal cord compression), misdiagnosis is common and often fatal. With this in mind, physicians and medical teams must be wary of the potential of NF, especially since there is not always a clear symptom that may point to necrotizing fasciitis at initial onset. Patients presenting with disproportionate pain related to physical findings and other systemic symptoms should be high on the clinical index of potential NF.6,7
Early recognition of critical imaging findings, such as subcutaneous and intramuscular air on CT scans, is paramount in considering necrotizing fasciitis within the differential diagnosis. Integration of imaging findings and clinical judgment should prompt further investigation if NF is suspected in any form.8 In our case, further investigation in the form of clinical observation, laboratory assessments, and progressive imaging studies yielded a successful diagnosis and outcome, as is seen in other cases in the literature.9,10
The cornerstone of treatment for necrotizing fasciitis is early surgical debridement. Our patient required multiple surgical procedures to remove all necrotic tissue. Continuous surveillance of the surgical wounds for signs of infection, along with the early removal of eschar, was necessary to promote adequate wound healing and lessen the potential for reinfection. The literature supports that timely surgical intervention is one of the most effective procedures that correlates with better outcomes. Delays in surgical intervention can lead to irreversible tissue damage, increased risk of systemic complications, and increased mortality.11,12
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.