Introduction
CLL is a hematological malignancy characterized by the uncontrolled proliferation of mature, neoplastic B-cell lymphocytes throughout the blood, bone marrow, lymph nodes, and spleen.1 Chronic lymphocytic leukemia is one of the most common types of leukemia, more commonly seen in older adults, with over 90% of those affected being 45 years of age or older with the median age of 72 years.2 There are four common chromosomal mutations that are associated with the majority of CLL patients: a deletion of 11q, 13q, 17p, or trisomy 12.3 The tumor suppressor gene TP53 is found within 17p and mutations of this gene are associated with up to 37% of CLL patients who often have a very poor prognosis.4 The immunophenotype of CLL shows expression of CD5 as well as B-cell antigens CD19, CD20, and CD23.5,6 Diagnosis requires a presence of greater than 5000 B-lymphocytes/μL for 3 months. CLL cells on blood smear appear as small, mature lymphocytes with a dense nucleus missing identifiable nucleoli, containing partially aggregated chromatin, and scant cytoplasm.1 The development of CLL to a more aggressive lymphoma, such as B-cell lymphoma (BCL), is known as Richter’s syndrome (RS) and affects up to 15% of CLL patients.7,8 BCL is the most common subtype of Non-Hodgkin’s Lymphoma (NHL), but is rarely present as a pedal neoplasm.9,10 In this report, we present a case of a 76 year old male with CLL who presented to the emergency department (ED) for eye swelling, but upon further physical examination, was referred to podiatry for a consult due to multiple ingrown toenails and potential onychomycosis.
Case Presentation
A 76-year-old male with a history of chronic lymphocytic leukemia (CLL), hypertension, hyperlipidemia, and gastroesophageal reflux disease (GERD) presented to the ED with left periorbital edema and erythema that developed after yard work 3 days prior and has been worsening. Initial evaluation revealed an elevated white blood cell count, raising concern for infection. The patient reported a longstanding history of chronic inflammation and recurrent infections of his toenails, characterized by ingrowth, intermittent drainage, and hypertrophy of nail folds. The patient was diagnosed with left periorbital/preseptal cellulitis with an associated abscess. After being admitted, he was seen by ophthalmology and infectious disease who prescribed aggressive IV antibiotics and abscess drainage. He presented with a right great toe infection that was later submitted for wound culture and came back with light growth of staphylococcus aureus. The day after coming to the ED, patient was seen by podiatry for evaluation of bilateral ingrown toenails with active infection and a history of biopsy-proven low-grade B-cell lymphoma (BCL) in the left third toe in 2019. The most concerning area was the right lateral hallux, which exhibited marked purulent drainage, eschar, and significant edema. Physical examination revealed edematous and tender nail folds bilaterally with hypertrophy due to the chronicity of the paronychial infection and the irritation of the nail against the skin. The left great toenail was also notably incurvated and painful to palpation. A nail avulsion procedure with I&D of the paronychial abscess was recommended for the right great toe, and the patient’s wife provided a 2019 pathology report confirming BCL in the left third toe.
The next day, he underwent incision and drainage of the left lacrimal duct abscess with packing. Purulence was encountered in the area of the lacrimal sac and lacrimal crest, and cultures were sent. Postoperatively, there were no signs of orbital involvement, and the patient exhibited normal ocular motility and optic nerve function. Microbiology results later revealed heavy growth of Staphylococcus aureus with inducible clindamycin resistance. The patient was started on intravenous vancomycin and cefepime for infection control and monitored for any signs of orbital extension.
The day following incision and drainage of the left eye abscess, the patient underwent a nail avulsion and I&D of the right hallux abscess, accompanied by a 2mm punch biopsy of the right great toe. The procedure revealed significant loosening of the medial nail and necessitated full nail avulsion. Pathology of the right toe confirmed low-grade BCL, with immunohistochemical staining showing PAX5 B cells with an immunophenotype CD3, CD5, CD10, CD21, CD23, BCL1, BCL2, BCL6 consistent with history of CLL transforming to BCL. FISH analysis demonstrated no cytogenetic abnormalities. Cultures from the toe revealed light growth of Staphylococcus aureus resistant to clindamycin.
The patient reported mild pain and bleeding postoperatively, with no signs of ascending cellulitis or lymphangitis. The care plan included mupirocin gauze dressing twice daily and continuation of IV antibiotics under infectious disease guidance. Follow-up evaluation at outpatient wound care center revealed the right hallux was healed, with no further drainage or wound care required. Biopsy findings confirmed recurrent BCL in the right great toe. The rare manifestation of CLL transforming into BCL in distal nail folds was discussed with the patient and his wife. Photos were taken to document healing, and consent was obtained for potential journal publication of this unique presentation. The care team reviewed the course and outcomes, emphasizing the multidisciplinary approach required to manage such complex cases.
Discussion
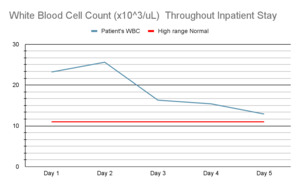
Along with the initial complete blood count showing high WBC and high atypical lymphocytes, there was a low neutrophil percentage. The patient was admitted for five days in the hospital. Throughout his stay in the hospital, six abnormal lab values were identified: WBC, neutrophil percentage, atypical lymphocytes, glucose serum, and AST. From days one to five, the patient’s abnormally high WBC count progressively declined as he received treatment: Day 1 (23.2 103/uL), Day 2 (25.6 103/uL), Day 3 (16.3 103/uL), Day 4 (15.4 103/uL), Day 5 (12.9 103/uL). Glucose was measured on three times throughout his hospital stay: Day 1 (111 mcg/dl), Day 2 (106 mcg/dl), Day 4 (112 mcg/dl). AST was only measured on the first and second day of the patient’s hospital stay: Day 1 (9 U/L), Day 2 (11 U/L). Neutrophil percentage (27%) and atypical lymphocyte percentage (17%) were low and high respectively on Day 1 in the hospital. eGFR went from a low value (57 mcL/mn) to normal (>60 mcL/mn) between day 1 and day 4 of the patient’s stay. Patients diagnosed with CLL typically have neutropenia, and the neutrophils in these patients likely have decreased response to pathogens.11 Patient’s leukocytosis is consistent with known history of CLL.12 Measurements of the left second toe wound showed a total area of 2.12cm2, length of 1.54cm, width of 2.22cm, and perimeter of 7.59cm.
A patient with low neutrophil count may have compromised innate immune system function.13 Neutropenia may suggest patient’s increased risk to bacterial Staphylococcus aureus infection of the lacrimal duct due to decreased number of neutrophils and efficacy of phagocytosis and creation of reactive oxygen species to eliminate microbes.11 Complete blood count showed increased WBC, or leukocytosis, with increased atypical lymphocytes. Leukocytosis may be indicative of ongoing infection, inflammation, and leukemic neoplasia.12 Neutrophils are the primary responders for initiating and maintaining immune mechanisms against infection.13 Leukocytosis is consistent with patients known history of CLL, and active Staphylococcus aureus infection with inflammation of the left periorbital area. Increased value of atypical lymphocytes are also consistent with patients’ known history of CLL.
Typical presentations of patients with CLL include lymphocytosis on a complete blood count with unknown etiology.14 This patient did not present with lymphocytosis, however he did have increased WBC with a predominance of atypical lymphocytes. Patient’s immunophenotyping showed PAX5 B cells- positive for CD23, CD5, CD21, BCL 1, BCL2, BCL6 that are classic for CLL and BCL. This is a unique case of CLL due to the rare occurrence of extranodal CLL in the skin- as reported in a systematic search for English language articles between 2000 and 2019 identifying 56 cases.15 This rarity is confounded with the histological transformation into BCL as reported in the biopsy.16 Differential diagnoses for this patient included vasculitis, squamous cell carcinoma, basal cell carcinoma, melanoma, cutaneous bacterial or fungal abscess and given this patient’s history, lymphoma.
Nail avulsion was performed based on the appearance of the toe that looked like an ingrown nail with paronychia. Oral or parenteral antibiotics are generally not part of the standard of care for an uncomplicated ingrown nail infection because the infection is highly localized. The nail had lacerated the nail groove causing an open wound susceptible to infection. When the nail plate was removed, the skin was able to begin the healing process because it was no longer aggravated by the nail acting as a contaminated foreign body. A biopsy was taken because the hallux maintained an atypical appearance following the removal of the nail that prompted concern.
In this case, the provider had initially recommended glucocorticosteroid injection treatment around the affected site status post nail avulsion. The patient had reported previous usage of topical steroids with poor efficacy and the provider’s decision was to move forward with dilute chlorhexidine soaks. This local treatment for the extranodal CLL to BCL transformation is to address possible infection.
This case is an excellent example for physicians to not overlook the distal extremities. With any treatment or consideration for a procedure, one must look at the complete clinical picture. Conditions affecting the toes can often affect the fingers.17,18 The right 3rd finger of this patient had some atypical swelling at the eponychium. Of note, conditions of the fingers may look slightly different as they are not subject to the chronic microtrauma of toes from walking and shoegear.
Conclusion
BCL can occur secondary to CLL with neoplastic cells having the potential to spread to any organ system in the body, including the distal extremities. In this case, a man in his 70s with CLL experienced presented to the ED with eye pain and swelling after yard work. Upon further examination of his feet, podiatry was consulted to assess his condition. Right greater toe avulsion was done and a biopsy was taken, showing diffuse large B cells confirming a diagnosis of BCL. Upon follow up, the patient was recovering from the procedure well. This case demonstrates a rare occurrence of CLL progressing to BCL in the distal extremities. Additionally, this case emphasizes the need for thorough examination of the distal extremities and digits to ensure pathologies unassociated with a patient’s chief concern are not missed. This case report contributes to the existing knowledge of CLL presentation and how it can develop into a more malignant BCL in various anatomical regions. Further research is necessary to explore the mechanisms and patient outcomes regarding the progression of CLL.
Ethical Considerations
Written informed consent was obtained from the patient for publication of this case report.