Introduction
Ifosfamide, an alkylating agent similar to cyclophosphamide, is utilized either alone or alongside other drugs. This cytotoxic and antineoplastic drug is used in treating a range of cancers, including lymphoma, sarcoma, and germ cell tumors.1 However, its use can lead to severe side effects, such as hemorrhagic cystitis, nephrotoxicity, myelosuppression, and neurotoxicity, especially ifosfamide-induced encephalopathy (IIE).
Ifosfamide, in its original state, is an inert prodrug that remains inactive until it undergoes hepatic metabolism, a process orchestrated by the CYP450 enzymes. This metabolic conversion generates active metabolites, including phosphoramide mustard derivatives, acrolein, and chloroacetaldehyde. Notably, chloroacetaldehyde has been implicated in the onset of ifosfamide-induced encephalopathy (IIE), which is attributable to its ability to traverse the blood-brain barrier. This is compounded by its structural resemblance to compounds like chloral hydrate and ethanol, both of which are recognized for their central nervous system (CNS) activity2
Although cyclophosphamide and ifosfamide share a close structural relationship, cyclophosphamide has not been associated with neurotoxicity. This distinction arises chiefly from the slower metabolic processing of ifosfamide, which consequently prolongs the body’s exposure to its metabolites3 When administered at elevated doses ranging from 3800 to 5000 mg/m², the drug has a half-life of approximately 15 hours. In contrast, at lower doses between 1800 and 2400 mg/m², its half-life is reduced approximately 7 hours. The primary pathway for drug elimination is renal filtration, making it crucial to adjust dosages according to the patient’s renal function to ensure safe and effective treatment4
The most frequently observed symptoms encompass a spectrum from somnolence, confusion, and depressive psychosis, to agitation, hallucinations, extrapyramidal manifestations, convulsions, and, in severe cases, coma or even death. This adverse reaction can occur anywhere between 2 and 96 hours following drug administration1
IIE is primarily diagnosed through clinical evaluation, necessitating advanced practitioners to thoroughly rule out other potential causes of encephalopathy, such as infections or metabolic abnormalities. Management of IIE typically involves discontinuing the infusion, ensuring adequate hydration, and administering reversal agents such as albumin, thiamine, and methylene blue (MB). However, there are documented instances where encephalopathy has resolved spontaneously, generally within 2 to 3 days following the cessation of ifosfamide5 and the likelihood of ifosfamide being the causative agent is evaluated via the Naranjo Adverse Drug Reactions (ADR) probability scale.6
The aim of this paper was to report our experience with ifosfamide-induced encephalopathy, its risk factors to highlight the preventive measures and therapeutic strategies for IIE.
Case presentation
Case 1
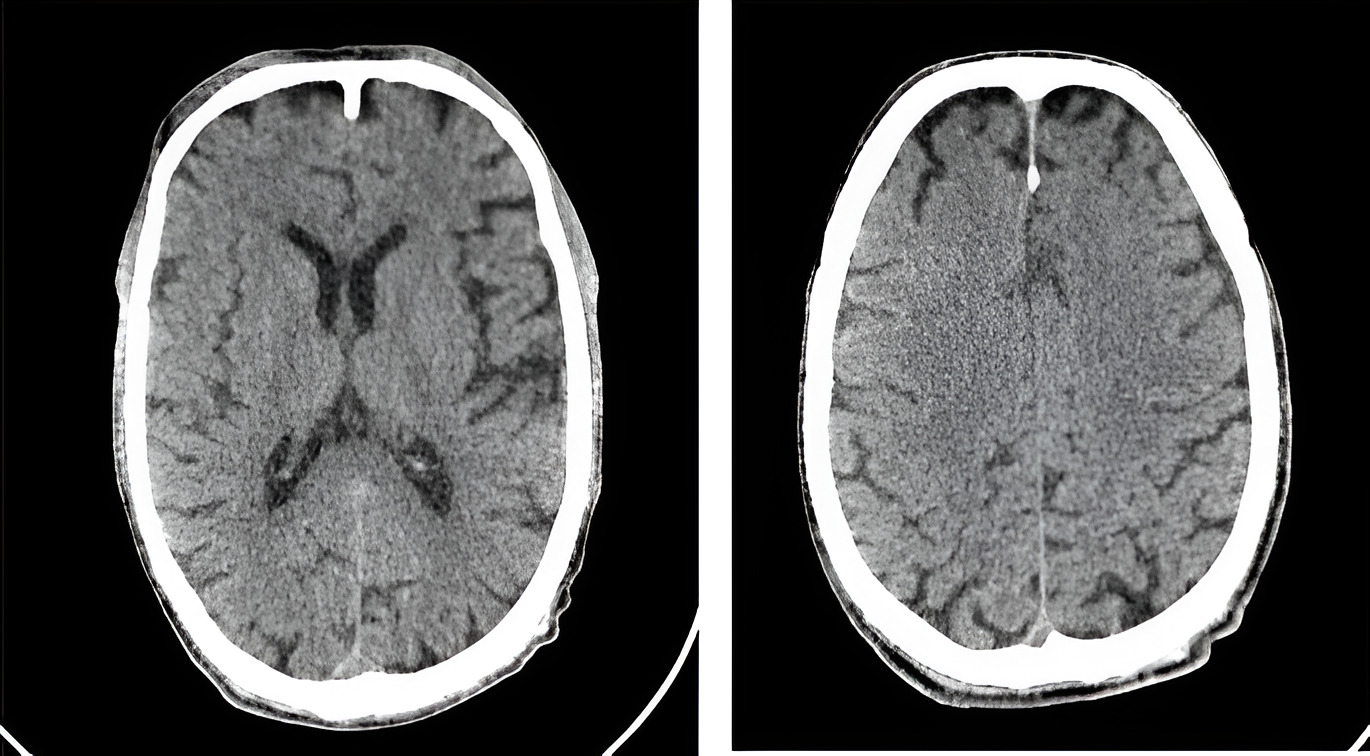
The brain CT images demonstrate a normal appearance of the cerebral hemispheres, ventricles, basal ganglia, thalami, brainstem, and cerebellum, with no evidence of acute pathology or structural abnormalities.
We present the case of a 62-year-old male with no notable past medical history who was recently diagnosed with synovial pleural sarcoma. Upon initial evaluation, the patient was found to have an Eastern Cooperative Oncology Group (ECOG) performance status of 2.7 Clinically, he was largely asymptomatic, except for grade II dyspnea and generalized fatigue. A comprehensive physical examination revealed no significant abnormalities.
The patient was admitted to our department for the initiation of his first chemotherapy cycle, consisting of Ifosfamide and Doxorubicin. Baseline laboratory investigations, including hematological and biochemical panels, were within normal limits (table 1), and cardiac function assessment yielded no contraindications to the proposed regimen. Consequently, we commenced systemic chemotherapy with intravenous administration of Doxorubicin at a dose of 75 mg/m2 every 21 days, alongside Ifosfamide at a dose of 3 g/m2 per day over a 2-3-day period, also on a 21-day cycle.
However, on the first day of chemotherapy administration, the patient exhibited signs of neurological toxicity, characterized primarily by excessive somnolence and episodes of disorientation. An urgent brain CT scan, along with an extended panel of laboratory tests, was conducted, yet no structural or metabolic abnormalities were identified (figure 1). In light of these findings, the infusion of Ifosfamide was immediately discontinued. Supportive management with aggressive intravenous hydration alone resulted in complete resolution of the neurological symptoms, as documented in (Table 2).
Case 2
No acute pathological findings or structural abnormalities are identified in the patient’s CT images.
We present the case of a 68-year-old male with a significant medical history, including type 2 diabetes mellitus (T2DM), ischemic cardiopathy, and a previous cardiac bypass, who was admitted to our department following a diagnosis of large retroperitoneal liposarcoma. On initial evaluation, the patient was found to have an Eastern Cooperative Oncology Group (ECOG) performance status of 2. Clinical examination revealed the presence of moderate ascites, accompanied by edema involving the scrotum and lower extremities.
Given the advanced nature of the malignancy, the multidisciplinary team opted for a palliative chemotherapy regimen consisting of Doxorubicin and Ifosfamide. In light of the patient’s pre-existing cardiac history, a detailed consultation was undertaken with the cardiology team. It was agreed that the patient would undergo regular and meticulous monitoring of cardiac function throughout the treatment course to preemptively address any potential complications. Additionally, the patient was initiated on diuretic therapy for the management of fluid retention. Initial laboratory investigations were within the normal limits (Table 1).
On the second day of Ifosfamide administration, the patient developed significant agitation, necessitating the use of benzodiazepines; diazepam at a dose of 0.2mg/kg administered as a slow IV and repeated twice for symptomatic management. Consequently, the infusion of Ifosfamide was discontinued, and aggressive hydration was initiated to correct potential renal dysfunction while maintaining vigilant monitoring of both cardiac and renal parameters. Despite these measures, a head CT scan and laboratory investigations conducted at this juncture revealed no structural or biochemical abnormalities (figure 2) (Table 2).
The patient’s clinical condition deteriorated further, marked by a progressive decline in the Glasgow Coma Scale (GCS) score, ultimately resulting in a comatose state. Despite the implementation of intensive supportive measures, such as methylene blue; the patient’s condition continued to worsen, and died two days later.
Discussion
The incidence of neurological toxicity from IFO varies widely from 10-40 % in adults1 and 2-30% in pediatric patients8
Demographic factors such as age and sex appear to have minimal effects on this neurological toxicity. Advanced age, particularly over 65 years as noted by Kettle and colleagues,9 may be partially linked to a heightened risk of dehydration, compromised renal function, and hypoalbuminemia. While female sex has been associated with lower body weight in several risk factor studies, no significant causal relationship has been established.
The clinical manifestations of ifosfamide-induced neurological toxicity can vary from drowsiness and confusion to hallucinations, seizures, and coma, with severe cases potentially resulting in mortality, particularly in pediatric patients10
The National Cancer Institute has classified IIE into 4 grades : Grade 1- vague or slightly depressive affect, Grade 2— extensive periods of sleep, restlessness or agitation, Grade 3— stupor, heavy depression or mild hallucinations; and Grade 4— vert hallucinations, seizures or coma11
While IIE is typically observed during the initial cycles of ifosfamide administration, occurrences in subsequent cycles are also documented. For example, Sweiss and colleagues have reported cases where symptoms persisted until the third or fifth cycle of treatment12
While there is insufficient evidence that a history of IIE is a risk factor for its occurrence in later cycles, it is still portrayed as one of the items in the adverse reaction assessment proposed by Naranjo.6
Compelling evidence both univariate and multivariate analyses from Lo and colleagues, demonstrated that a performance status (ECOG) of 2 or higher confers a 5.15-fold increased risk of developing ifosfamide induced encephalopathy compared with patients with a performance status (ECOG) of 0-1. This finding aligns with our own results13
Ifosfamide is metabolized in the liver through the action of CYP450 enzymes, resulting in the formation of its active metabolites.4 Interactions with CYP3A4 inducers, such as phenobarbital, carbamazepine, and phenytoin, have been investigated, yet no statistically significant differences were detected.14
The presence of brain metastases has been identified as a potential predispositional factor; however, given that brain metastases occur in less than 3% of cases involving soft tissue sarcomas, they are regarded as an infrequent mechanism of neurotoxicity within this patient population and should be considered more as a differential diagnosis15
Impaired liver function—given the substantial hepatic metabolism of ifosfamide—was not a significant factor in the development of IIE according to the literature.16 Instead, renal insufficiency emerged as the most frequently cited risk factor, attributed to the reduced clearance of neurotoxic metabolites. This aligns with the findings of the most extensive study conducted by Lo and colleagues, which included 337 patients13
Similarly, an elevated tumor burden, particularly involving pelvic malignancies, may be a potential risk factor for IIE, such conditions can contribute to urinary obstruction and impaired drug elimination, as exemplified by one of our patients who had a substantial retroperitoneal liposarcoma. This tumor caused compression of the inferior vena cava (IVC) and led to minimal unilateral ureterohydronephrosis.
Like all other biomarkers derived from peripheral blood, albumin levels are markedly influenced by inflammatory conditions. A reduction of its levels is often observed in chronic inflammatory disorders and malignancies. Numerous studies involving patients undergoing chemotherapy, radiotherapy, or targeted therapies have indicated that diminished albumin levels are associated with an increased risk of mortality or disease progression, as well as a higher incidence of toxicity17
Patients with hypoalbuminemia (commonly defined as serum albumin levels less than 3.5 g/dl) tend to experience more severe chemotherapy-induced toxicity symptoms, attributed to the elevated concentration of unbound drug in the systemic circulation.16 In a retrospective study by Kettle and colleagues, the potential protective effect of improving serum albumin levels was explored. However, contrary to expectations, the incidence of IIE was greater in the group receiving albumin perfusions, indicating that this approach may not be an effective preventive strategy9
Risk factors, including the dosage, duration, and frequency of ifosfamide infusions, were investigated in relation to treatment characteristics. Richards and colleagues identified several key risk factors for the development of IIE, specifically an infusion time of 1 to 2 hours, a total ifosfamide dose per cycle of 8 g/m² or greater, and an administration frequency of every 12 hours.
These conditions are rare in the literature and among our patients, as the majority of reported cases exhibit symptoms during the first cycle of administration, typically at doses less than 3 g/m², as observed in our two cases. While ifosfamide is classified as a moderate-to-severe emetogenic agent by various medical societies, the concurrent use of aprepitant is a common practice in most polychemotherapy regimens. This combination was highlighted in one case study as a potential risk factor for IIE, and a systematic review suggested a positive relationship between neurotoxicity and the concomitant use of ifosfamide with aprepitant or fosaprepitant. However, this association did not reach statistical significance18
The influence of other chemotherapeutic agents was observed mainly with cisplatin.
Its concomitant use with ifosfamide, is a possible risk factor for IIE due to the cumulative renal tubular injury, this coadministration of ifosfamide with cisplatin was illustrated by Ide and colleagues’ study exclusively in the pediatric population.
However, the previous administration of cisplatin and the increase in creatine serum levels were indicated in multiple adult cohorts as factors enhancing ifosfamide mediated nephrotoxicity19
Hence, we need to closely monitor serum creatinine levels in adult patients who are under or have been receiving a chemotherapy cisplatin-based regimen and to avoid the association of CDDP and IFO in the pediatric population as much as possible.
Despite the notable incidence of IIE, no treatment has been conclusively proven to reverse its neurotoxicity. Preventive strategies, such as thiamine prophylaxis—considering the similarity between ifosfamide-induced neurological effects and Wernicke’s encephalopathy, which results from severe thiamine deficiency—and the use of albumin, or a combination of these, have not been associated with a reduced incidence of IIE in retrospective analyses.16
The primary limitation of this analysis lies in the self-limiting nature of IIE, making establishing a direct connection between these preventive measures and a reduction in incidence challenging.
The main immediate measures are the discontinuation of ifosfamide perfusion, an adequate hydration is usually an effective measure for early diagnosis mostly mild IIE cases and, by extension, most chemotherapy-induced toxicities.
For reversal agents, intravenous administration of methylene blue at a dosage of 50 mg every four hours has been documented to be effective in counteracting neurotoxicity.16 Indeed, a review of the literature revealed that 65.5% of IIE cases were treated with methylene blue as a neurotoxicity-reversing agent, with a successful reversal observed in 75% of the reported cases1
Methylene blue (MB) is believed to influence several metabolic pathways implicated in ifosfamide-induced encephalopathy.20 It functions as an alternative electron acceptor to prevent the accumulation of chloroethylamine and inhibits both plasma and and extrahepatic monoamine oxidases, thereby reducing the buildup of chloroacetaldehyde, which can cross the blood‒brain barrier, resulting in IIE symptoms; however, the use of MB remains contentious, as its efficacy has yet to be fully substantiated.20 The treatment dose is set at 50 mg and is administered intravenously or orally, either as a single dose or every 4 to 8 hours until symptoms abate. For prophylaxis, the dosage is 50 mg intravenously or orally every 6 to 8 hours throughout the duration of ifosfamide infusion.21
Conclusion
Ifosfamide, an alkylating agent, is known for inducing both acute and delayed neurological complications, with encephalopathy being one of its most severe side effects. The vigilance of healthcare professionals, alongside fundamental management strategies—such as ensuring adequate intravenous hydration, administering methylene blue or thiamine, and conducting hourly neurological assessments—remains the cornerstone of effective intervention.
Although no miraculous reversal therapy exists, evaluating these risk factors and educating patient’s caregivers about potential side effects enables improved patient counseling and close monitoring of those at risk.
Ethics approval
The authors’ institution does not require Ethics Committee approval for the publication of case reports.
Availability of data and material
The datasets used and analyzed during the current study are available from the corresponding author.
Competing interests
The authors declare no competing interests related to this study
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Authors’ contributions
All authors contributed equally to the conception, design, data collection, analysis, and writing of this manuscript
Acknowledgments
The authors thank the archive team and the pharmacovigilance unit.
List of abbreviations
STSs: soft tissue sarcomas
IIE: Ifosfamide-induced encephalopathy
MB: methylene Blue
CNS: central nervous system
ECOG: Eastern Cooperative Oncology Group
IVC: inferior vena cava
G6PD: glucose-6- phosphate dehydrogenase