Introduction
Adolescent idiopathic scoliosis (AIS) is the most prevalent form of scoliosis, predominantly affecting individuals aged 10 to 18 years.1 A diagnosis of AIS is confirmed when the Cobb angle measures 10° or greater and is accompanied by vertebral rotation.1 AIS manifests as a three-dimensional spinal deformity with an unknown etiology.2 Although many theories have been proposed with regard to the etiology of AIS including hormonal imbalance, asymmetric growth, and muscle imbalance, the exact cause remains unknown.3 While many cases of AIS are mild and do not necessitate intervention, some patients develop a progressive spinal curvature that can lead to significant physical deformity, which, if left inadequately treated, may result in both physical and psychological challenges.4 The long-term effects of inadequately treated AIS include severe pain, cardiopulmonary compromise, social isolation, respiratory dysfunction, diminished quality of life, and increased risk of premature mortality.5
Therapeutic interventions for AIS are specifically tailored for each patient based on the severity of the spinal curvature and their level of skeletal maturity.6 Minimally invasive treatments, such as bracing, physical therapy, and physiotherapeutic scoliosis-specific exercises (PSSE) are utilized to treat mild to moderate spinal curvature.6 However, surgical intervention becomes necessary in cases where the curvature progresses or symptoms worsen despite these conservative treatment approaches. Surgical correction restores spinal alignment, prevents further progression of curvature, and alleviates any associated symptoms to ultimately improve overall structure, function, and quality of life. Posterior spinal fusion with instrumentation is the standard surgical approach for correcting AIS. This surgical intervention achieves substantial spinal curvature correction while preserving cosmetic appearance and functional outcome, resulting in improved patient satisfaction and quality of life.7
This case report presents a 13-year-old female patient with severe AIS, detailing her clinical presentation, the surgical correction performed, and her outcomes at the time of this study.
Case Presentation
The patient is a 13-year-old female presenting with a chief complaint of progressive left-sided spinal curvature [Figure 1]. Over the past three years, the curvature had progressively worsened despite undergoing physical therapy, which showed no significant improvement. She also reported experiencing pain and observed increased prominence of her left shoulder blade over time.
On examination, the patient was fully alert, oriented, and hemodynamically stable, with a normal blood pressure, pulse, temperature, and respiratory rate. Further assessment revealed left-sided thoracic scoliosis, accompanied by a pronounced asymmetry of the shoulder blade. While mild spinal deformity was evident, there was no associated neurological deficit or focal neurodeficit. The patient had no significant medical history and denied any allergies to medications or other substances.
Diagnostic Assessment
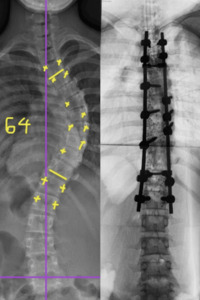
Diagnostic imaging played a crucial role in evaluating the severity of the patient’s scoliosis. Preoperative X-rays, obtained using EOS imaging, revealed a thoracic Cobb angle of 64° and a lumbar Cobb angle of 39°, indicating a severe degree of spinal curvature [Figure 2]. These findings confirmed the diagnosis of adolescent idiopathic scoliosis (AIS), characterized by a pronounced thoracic curvature. AIS is a common condition in adolescents, defined as an idiopathic lateral curvature of the spine that develops during the growth period.8
Treatment
Given the severity of the spinal curvature and the patient’s poor response to conservative measures, surgery became unavoidable. The treatment involved posterior spinal fusion with instrumentation. The patient was positioned prone during the procedure, and neurophysiological monitoring was employed to continuously assess spinal cord function.9
The postoperative management of this patient involved close monitoring in the intensive care unit (ICU) during the first 24 hours following surgery. Pain management was a critical component to mitigate potential adverse events and was effectively addressed with analgesics. Follow-up radiographic assessments demonstrated a satisfactory correction of the spinal deformity, with the thoracic Cobb angle reduced to approximately 15 degrees and the lumbar Cobb angle to 10 degrees [Figures 3-4].
Results and Outcomes
Postoperative radiologic evaluation confirmed the efficacy of the surgical treatment, with significant improvement observed in the thoracic and lumbar spine. The thoracic Cobb angle was reduced to 15 degrees, and the lumbar Cobb angle to 10 degrees. These changes, based on the criteria used, represented favorable corrections of the spinal curvature.
Clinically, there were no complications or signs of deterioration in the patient’s condition. She was discharged in good health on the fifth postoperative day. At a follow-up two months after surgery, the patient reported minimal discomfort, significant improvement in the surgical scar, and noticeable relief. She quickly adopted a correct sitting posture and expressed feeling comfortable and at ease, underscoring the success of the surgical intervention.
Discussion
This case underscores the critical importance of early diagnosis and timely surgical intervention in adolescents with severe AIS.10 In this case, posterior spinal fusion with instrumentation was shown to effectively correct spinal deformity while minimizing postoperative complications, aligning with previous research findings.11 Additionally, neurophysiological intraoperative monitoring was instrumental in preventing neurological adverse effects during the procedure.12
Despite attempts with various conservative measures to halt the progression of the curve, surgery became necessary when these efforts proved ineffective. The outcome of this case demonstrates that surgical intervention in severe AIS can lead to significant improvements in both the patient’s physical and mental well-being.13
This case highlights the vital role of teamwork, involving orthopedic surgeons, anesthetists, and rehabilitation specialists. Interdisciplinary collaboration plays a crucial role in ensuring comprehensive care, from accurate preoperative diagnosis to tailored postoperative rehabilitation. This approach enhances the effectiveness of surgical intervention, streamlining the recovery process and improving the patient’s long-term quality of life.14
Furthermore, this case highlights the significant psychosocial benefits of surgical intervention for adolescents with severe scoliosis. Psychological challenges, such as body image disturbances, low self-esteem, and self-consciousness due to visible deformities, are common among AIS patients.15 This report demonstrates how successful correction of spinal curvature positively impacted this patient’s self-image and self-confidence, emphasizing the importance of addressing these aspects as integral components of AIS treatment.16 Early psychological support, both before and after surgery, played a crucial role in helping the patient come to terms with the physical changes associated with the procedure.17 Effective scoliosis treatment must address both the physical and emotional needs of the patient, underscoring the necessity of a patient-centered approach to care.
Conclusions
Surgical correction of severe scoliosis in adolescents is highly effective in restoring spinal alignment and significantly improving patients’ quality of life, functional outcomes, and physical appearance. This case report highlights the crucial role of timely surgical intervention and the efficacy of posterior spinal fusion with instrumentation in achieving substantial curvature correction and preventing further progression. The successful outcome of this patient underscores the importance of a multidisciplinary approach, integrating meticulous preoperative planning, precise surgical techniques, and structured postoperative rehabilitation. These findings reinforce the necessity of individualized, patient-centered care in the management of severe AIS, ensuring optimal clinical and psychological outcomes.
Ethical considerations
The patient provided written informed consent for this case report.