Introduction
Fecal incontinence (FI), characterized by the involuntary loss of fecal matter, affects 7-15% of adults, disproportionately impacting women with a history of obstetric anal sphincter injuries (OASIs).1–3 OASIs, which occur in 0.5-11% of vaginal deliveries depending on obstetric practices, are the leading cause of FI and often result from factors such as instrumental delivery, prolonged labor, primiparity, and high birth weight.4–8 Despite primary repairs, 20-40% of women develop persistent FI symptoms, with 10-50% experiencing complications like infections, wound dehiscence, or impaired sphincter function.9–12
Secondary overlapping sphincteroplasty is the preferred surgical intervention for persistent FI due to its better functional outcomes than end-to-end repair.13–15 Success rates vary, with continence restored in 50-85% of cases at 1-10 years, though recurrence rates range from 30-50%.16–22 Adjunct therapies such as sacral nerve stimulation and biofeedback have shown promise, but their limitations warrant further evaluation.23–25
From a colorectal perspective, secondary overlapping sphincteroplasty addresses severe sphincter disruptions caused by OASIs, but challenges remain, including suboptimal sphincter function post-repair, recurrence of symptoms, and potential long-term colorectal complications like rectal prolapse or chronic constipation.26,27 Approximately 40% of women with unresolved FI undergo secondary sphincteroplasty, highlighting the need for a comprehensive assessment of its efficacy and safety, with an emphasis on long-term colorectal outcomes.20,28,29
Objectives
-
To provide an overview of the effectiveness of sphincteroplasty in managing fecal incontinence in patients with obstetric anal sphincter injuries.
-
To discuss the reported long-term outcomes of overlapping versus end-to-end sphincter repair techniques.
-
To explore how patient-related factors, surgical techniques, and postoperative rehabilitation influence treatment outcomes.
-
To examine the potential role of adjunctive therapies, such as sacral nerve stimulation, in enhancing continence and quality of life.
Methods
Study Design
This systematic review adhered to PRISMA guidelines and the principles of comprehensive literature synthesis and qualitative analysis, aiming to provide a detailed overview of obstetric anal sphincter injuries (OASIs) and secondary overlapping sphincteroplasty outcomes.
Literature Search Strategy
A targeted literature search was conducted in electronic databases, including MEDLINE (PubMed), Embase, Cochrane Library, and Scopus, to identify relevant studies published up to November 2024. The search strategy used the following keywords and Medical Subject Headings (MeSH) terms such as “Obstetric anal sphincter injury,” “OASIs,” “Secondary sphincteroplasty,” “Overlapping sphincteroplasty,” “Fecal incontinence,” and “Anal sphincter repair.”
Study Selection
Articles were selected based on their relevance to the objectives of this review. Studies were considered if they provided data on the management of OASIs, particularly secondary overlapping sphincteroplasty, focusing on functional outcomes, quality of life, or complication rates. Emphasis was placed on articles describing surgical techniques, outcomes, or rehabilitation approaches.
Inclusion and Exclusion Criteria
Inclusion Criteria
-
Studies discussing obstetric anal sphincter injuries and their management: These studies provide essential background information on OASIs, their risk factors, and current treatment approaches, forming the foundation of this review.
-
Reports evaluating secondary overlapping sphincteroplasty outcomes: Since this review’s primary focus is on the effectiveness of secondary overlapping sphincteroplasty, including these studies ensures that the review remains relevant and clinically applicable.
-
Articles detailing functional outcomes, quality of life, or complication rates: Articles detailing functional outcomes, quality of life, and Long-term patient-centered outcomes are critical in evaluating the success of secondary sphincteroplasty and guiding future clinical practice.
-
Studies across various designs, including randomized controlled trials, cohort studies, case series, and prior systematic reviews: A broad range of study designs allows for a comprehensive synthesis of evidence, as randomized controlled trials (RCTs) may be limited in this surgical field, while observational studies and systematic reviews provide valuable insights.
Exclusion Criteria
-
We excluded non-English articles without available translations: Language barriers can lead to misinterpretation of data, and excluding untranslated studies ensures the accuracy and reproducibility of findings.
-
Reports with incomplete or non-reproducible data: Studies with missing or unclear data may compromise the reliability of the review and hinder meaningful comparisons of outcomes.
-
Case reports with fewer than five patients: Small case reports lack statistical power and generalizability, limiting their contribution to robust evidence synthesis.
-
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRIMSA) diagram is depicted below [Figure 1].
Data Extraction
Data extracted from all articles which met inclusion criteria included:
-
Study characteristics: Publication details, design, and sample size.
-
Patient demographics: Age, parity, and mode of delivery.
-
Intervention details: Timing and type of sphincteroplasty, including overlapping versus end-to-end repairs.
-
Outcomes: Improvement in fecal incontinence, quality of life, complication rates, and recurrence of symptoms.
Quality Assessment
RCTs were assessed using the Cochrane Risk of Bias tool, and cohort and observational studies were assessed using the Newcastle-Ottawa Scale. Evidence was graded using GRADE.
Data Synthesis
Findings were synthesized thematically to provide insights into key areas, including:
-
Epidemiology, risk factors for OASIs, and classification of injuries.
-
Surgical approaches, with a focus on overlapping techniques.
-
Long-term outcomes, including functional recovery, recurrence, and quality of life.
-
Adjunctive therapies and rehabilitation strategies.
Ethical Considerations
This systematic review was based on a secondary analysis of published studies, so no ethical approval was required for the review. Patients provided informed consent for the photogarphs in figures 5-8.
The Review
Epidemiology of OASIs
Obstetric anal sphincter injuries (OASIs), encompassing third- and fourth-degree perineal tears, affect approximately 1-3% of vaginal deliveries globally.30,31 Incidence rates vary geographically, ranging from 1.4% in high-resource settings to 4-6% in low-resource regions.32,33 In Northern Europe, rates are higher due to stringent diagnostic and reporting practices.34,35 Additionally, a systematic review reported a 35% increase in OASIs rates over recent decades in developed countries, reflecting changes in obstetric practices and improved recognition.36,37
The condition has significant long-term consequences, with morbidity rates between 0.5% and 10%, depending on population demographics, obstetric care, and healthcare access.31,38 Among primiparous women, the incidence is as high as 6-8%, nearly double that of multiparous women.6,39
Risk Factors for OASIs
Several maternal, fetal, and obstetric factors contribute to the risk of OASIs. [Table 1]
Maternal Factors
-
Primiparity: First-time mothers are at a 60-80% higher risk than multiparous women, largely due to the absence of prior perineal stretching.40,41
-
Advanced Maternal Age: Women over 35 are more prone to OASIs due to reduced tissue elasticity.42,43
-
Short Perineal Body: A perineal body length under 3 cm increases OASIs risk by 45%.40,41
-
Obesity: Overweight and obese women face higher risks, likely due to increased perineal pressure and larger fetal sizes.44,45
Fetal Factors
-
Macrosomia: Birth weights exceeding 4 kg elevate the risk of OASIs by 2-3 times.46,47
-
Breech Presentation: Breech deliveries are associated with a nearly fourfold increase in OASIs risk compared to cephalic presentations.48,49
Obstetric Factors
-
Instrumental Vaginal Delivery:
-
Episiotomy:
-
Prolonged Second Stage of Labor: A second stage lasting over two hours increases the risk by 40%.57,58
-
Shoulder Dystocia: This complication further elevates the risk of severe perineal tears.41,59
-
Prior OASIs: Women with a history of OASIs face a 10-12% recurrence risk in subsequent deliveries.40,41
Preventive Strategies
Preventive measures include tailored delivery planning, training for healthcare providers, and controlled delivery techniques such as manual perineal support, which reduces the risk by 30%.9,53 Selective episiotomy and careful management of instrumental deliveries can also help mitigate the risk of OASIs.46,53,60 For high-risk cases, cesarean delivery may be considered.
This synthesis highlights the multifactorial nature of OASIs risk and the importance of recognizing and addressing modifiable factors to reduce its incidence and associated morbidity.
Classification and types of OASIs
The Sultan classification system is the most widely adopted and includes:
-
Grade 1 & 2: Perineal skin and superficial muscle involvement are seen in up to 65% of vaginal deliveries.52,56,61
-
Grade 3 (a-c): Partial or complete disruption of the external anal sphincter (EAS), affecting 45-60% of severe injuries.36,62
-
Grade 4: Complete rupture of both the EAS and internal anal sphincter (IAS) with rectal mucosal involvement, comprising 15-30% of cases.36,62
Emerging classification systems incorporating endoanal ultrasound aim to improve diagnostic precision.22,61 Another classification of OASIs includes partial and complete disruptions of the EAS and IAS. Fourth-degree injuries involving the rectal mucosa are the most severe, often leading to complications such as fecal incontinence, rectovaginal fistulas, and chronic pain if inadequately treated8,40,63
The Role of Clinical Assessment Versus Objective Investigations in OASIs Management
Clinical assessment using incontinence scoring systems, such as the Wexner and St. Mark’s Incontinence Scores, plays a vital role in evaluating the functional impact of OASIs. These tools assess symptoms like incontinence, urgency, and lifestyle interference, helping to stratify patients by symptom severity and guide management decisions. Studies show that up to 85% of patients with OASIs-related incontinence exhibit significant variability in symptom severity, highlighting the need for standardized assessments.2,32,62 However, these systems are based on patient-reported outcomes, which can be influenced by recall bias and social stigma.10,38
Objective assessments, including endoanal ultrasound (EAUS) and anal manometry, complement clinical evaluation by offering detailed anatomical and functional insights. EAUS, with a sensitivity of 85-95% for detecting sphincter injuries, is crucial for identifying defects and guiding surgical planning.1,53 Anal manometry provides information on sphincter pressure dynamics, revealing functional deficits that may not be clinically evident. Up to 30% of patients with low sphincter pressures on manometry show normal clinical scores, emphasizing the need for objective measures in routine assessment34,64,65
However, objective assessments have limitations, including the need for specialized equipment and expertise, which may not be available in resource-limited settings. A comparison of clinical scoring and EAUS revealed a 20% discrepancy in injury severity classification, suggesting that combining both approaches ensures a more accurate diagnosis and tailored management.58,66 While clinical scoring systems are helpful for initial assessments, integrating objective modalities like EAUS and manometry provides a more comprehensive evaluation, optimizing diagnosis, management, and outcomes for patients with OASIs.
Role of Imaging in the Evaluation of OASIs
Imaging is crucial in evaluating and managing Obstetric Anal Sphincter Injuries (OASIs), providing insights into both the anatomical damage and functional outcomes, as well as assessing the effectiveness of surgical interventions. Key modalities include endoanal ultrasound (EAUS), magnetic resonance imaging (MRI), and anal manometry.
Endoanal Ultrasound (EAUS)
EAUS is the gold standard for assessing anal sphincter integrity, with a sensitivity of 85-95% and specificity of up to 100% for detecting sphincter defects.57,64,67 It accurately identifies sphincter injuries in 85-90% of cases, particularly complete tears, and is valuable in post-surgery follow-up to detect recurrence or new injuries.67 Abnormal results were found in 15% of women post-repair, suggesting persistent or recurrent injuries.39
Magnetic Resonance Imaging (MRI)
MRI provides a broader view of pelvic structures, including the sphincters, levator ani, and puborectalis muscles, with a diagnostic accuracy of about 90% for OASIs.55 It is particularly useful when EAUS results are inconclusive or when a comprehensive view of the pelvic floor is needed. MRI also detects long-term complications, such as fibrosis, and influences surgical planning, with 30% of cases showing altered management based on preoperative MRI.5,68
Anal Manometry
Anal manometry assesses sphincter function by measuring anal pressures, providing essential data on strength and coordination. It is particularly useful for evaluating chronic fecal incontinence, with abnormal results found in 40% of women post-OASIs repair.69 Reduced anal pressures are associated with poorer long-term outcomes, including incontinence.69,70
Comparison and Integrated Use
Each modality offers unique strengths, and using them together enhances diagnostic accuracy by 15-20%, especially in complex cases involving multiple structures.13 EAUS identifies sphincter defects, MRI provides a broader anatomical view, and anal manometry evaluates functional status. The integration of EAUS, MRI, and anal manometry significantly improves the evaluation of OASIs, helping to guide management decisions, assess repair success, and predict long-term outcomes. As imaging technology evolves, its role in optimizing OASIs management and patient outcomes will continue to grow32,40,71
Management of Obstetric Anal Sphincter Injuries (OASIs)
Effective management of Obstetric Anal Sphincter Injuries (OASIs) is crucial to prevent long-term complications, such as fecal incontinence and pelvic floor dysfunction. Approaches include conservative management for mild injuries or early-stage care and surgical interventions for severe or persistent cases.
1. Conservative management
Conservative management focuses on symptom relief and rehabilitation, particularly for mild injuries or when surgical repair is delayed. Key strategies include:
-
Pelvic Floor Exercises (Kegel Exercises): Initiating Kegel exercises within six weeks postpartum strengthens the pelvic floor and anal sphincters, leading to a 70% resolution of mild incontinence symptoms.40
-
Biofeedback Therapy: This therapy improves anal sphincter function by providing real-time feedback during exercises. It has been shown to increase anal sphincter pressure by 30-40% in women with persistent fecal incontinence after OASIs.5
-
Stool Softeners and Dietary Modifications: To reduce strain during defecation, stool softeners, along with a high-fiber diet and increased fluid intake, help minimize constipation and prevent further sphincter injury.39
2. Surgical Management
Surgical treatment is indicated for more severe injuries or when conservative measures fail. The timing and techniques depend on the injury’s severity and chronicity.
Immediate Repair
Primary repair performed shortly after delivery is the standard approach:
-
End-to-end Repair: This method is utilized in 70-85% of cases and achieves anatomical restoration in over 90% of patients.30,46,72
-
Overlapping Sphincteroplasty: Preferred for complex injuries, overlapping sphincteroplasty improves continence in 65-75% of patients at one year.44,47,54
-
Suture Materials: Absorbable sutures, such as polyglycolic acid, are used in 80% of cases. They reduce infection rates by 20-25% compared to non-absorbable sutures.26,73
Secondary Repair
Secondary repair is performed when the primary repair fails, or symptoms persist:
-
Overlapping Sphincteroplasty: Secondary procedures relieve symptoms in 60-80% of patients, although long-term efficacy may decline.33,55,56,74
-
Complex Procedures: When the primary repair fails, colorectal surgeons may use advanced techniques like muscle flaps or overlapping repairs. Secondary sphincteroplasty improves continence in approximately 70% of cases.67
Emerging Techniques
New approaches show promise in managing refractory cases:
-
Stem Cell Therapy: Early studies suggest stem cells may aid in regenerating damaged tissues.32
-
Bulking Agents: Injectable agents improve anal sphincter bulk and function.75
-
Sacral Nerve Stimulation: This intervention enhances continence in patients unresponsive to conventional therapies.76
Comprehensive management tailored to the severity of OASIs is vital for restoring function, improving quality of life, and minimizing long-term complications.
Outcomes
The outcomes of OASIs are influenced by the severity of the injury, the quality and timing of repair, and long-term rehabilitation efforts. Management strategies aim to restore sphincter function, improve quality of life, and reduce complications through primary apposition repair or secondary overlapping sphincteroplasty.
Short-Term Complications of OASIs
In the immediate postpartum period, women with OASIs may experience physical complications such as:
-
Infections, Hemorrhagic Conditions, and Wound Dehiscence Occur in 4-10% of cases, and infections are the leading cause of delayed healing.38
-
Postoperative Pain and Bowel Dysfunction: These are common and often require dietary modifications, stool softeners, and analgesia, including prolonged opioid use.47,77
-
Fecal Incontinence and Urgency: Up to 20% of women report these symptoms within six months postpartum.47,77
Long-Term Complications of OASIs
The long-term impact includes
-
Fecal Incontinence and Sphincter Dysfunction: Persistent symptoms affect 20-40% of women years after delivery, influenced by the extent of injury and quality of repair.34,78,79
-
Sexual Dysfunction: Pain during intercourse (dyspareunia) and reduced satisfaction occurs in 40% of cases, significantly affecting the quality of life.5,34,78
-
Psychological Distress: Anxiety and depression are reported by 25-33% of women, often related to incontinence or pain.14,18,58
Timely intervention and rehabilitation involving multidisciplinary teams comprising colorectal surgeons, pelvic floor therapists, obstetricians, and mental health professionals are essential for improving recovery and long-term outcomes.5,22,80,81
Outcomes of Primary Apposition Repair vs. Secondary Overlapping Sphincteroplasty
OASIs management strategies include primary apposition repair (immediate) and secondary overlapping sphincteroplasty (delayed). Both techniques aim to restore sphincter integrity and function but differ in timing, approach, and outcomes.82,83 [Figures 2 and 3].
Primary Apposition Repair
Primary repair, performed shortly after delivery, involves direct end-to-end suturing of the sphincter muscles.
-
Short-Term Outcomes: Success rates range from 70% to 90%, with most women achieving satisfactory anal continence, especially when skilled obstetricians perform the repair promptly.54,56,84 Advanced maternal age and delayed recognition of injuries may reduce success rates.30,58,85
-
Long-Term Outcomes: Despite initial success, 30-50% of patients experience persistent or recurrent symptoms such as fecal incontinence. Contributing factors include sphincter degeneration, scarring, and inadequate healing.39,62,66 Regular follow-up is essential for high-risk patients.10,36,37
-
Complications: In some cases, wound dehiscence, infection, and perineal pain occur. Improved training of obstetricians can reduce these risks.34,69,77
Secondary Overlapping Sphincteroplasty
Secondary repair, performed months or years after delivery, is indicated for unresolved symptoms, chronic injuries, or failed primary maintenance. It involves overlapping the sphincter muscles for enhanced mechanical strength.
-
Short-Term Outcomes: Significant improvements in continence are seen in 60-80% of patients within the first year, particularly in chronic cases with CIs ranging from ±5% to 10%.2,57,61
-
Long-Term Outcomes: Continence rates decline to 40-60% over 5-10 years due to muscle atrophy, fibrosis, and nerve dysfunction, though many patients report improved quality of life.22,78,80,86,87
-
Complications and Reoperations: Infection, fistula formation, and perineal pain occur in 20% of cases, but reoperation rates are low when performed by experienced surgeons.20,35,41
-
Adjunct Therapies: Biofeedback and electrical stimulation enhance outcomes and patient satisfaction.24,67,69
Comparison of Primary and Secondary Repairs
-
Timing and Accessibility: Primary repair is performed immediately postpartum and is readily available, while secondary repair requires referral and longer recovery periods.66,68,88
-
Functional Outcomes: Secondary sphincteroplasty offers better structural reinforcement in chronic cases but shows diminishing efficacy over time due to tissue degeneration.6,22,35,62
-
Patient Selection: Primary repair is ideal for acute injuries, while secondary repair is reserved for women with unresolved symptoms, failed primary repairs, or significant sphincter disruption.13,57,89
Both approaches are critical in managing OASIs. Primary repairs are effective when performed promptly by skilled providers, whereas secondary overlapping sphincteroplasty addresses persistent symptoms or failed initial repairs. Optimal outcomes depend on careful patient selection, surgical expertise, long-term rehabilitation, and regular follow-up.5,12,77 Table 2 summarizes the techniques and outcomes.
Rehabilitation and Adjunctive Therapies
Rehabilitation and adjunctive therapies are integral to improving outcomes following OASIs. These approaches enhance recovery, restore function, and address psychological impacts.
Pelvic Floor Rehabilitation
-
Biofeedback Therapy: Strengthens pelvic floor muscles, improving muscle strength by 55% and enhancing anal sphincter tone. Some randomized controlled trials (RCTs) indicate a p-value <0.05 for these improvements, confirming their efficacy.2,85,86
-
Electrical Stimulation and Pelvic Floor Muscle Training: These techniques improve continence in 60% of patients with confidence intervals varying between ±8% and 12% and are key components of postoperative rehabilitation.2,85,86
Adjunctive Therapies
-
Topical Glyceryl Trinitrate: Increases wound healing rates by 20%, aiding recovery in the early postoperative period.8,64,85,86,90
-
Low-level laser therapy accelerates tissue healing and recovery, with promising results in clinical settings.8,64,85,86,90
Psychological Support
- Mental Health Interventions: Psychological impacts of OASIs, including trauma, anxiety, and depression, are common among affected women, and treatment has been shown to improve outcomes.8,20,28,91
Postoperative Rehabilitation
Postoperative rehabilitation strategies significantly improve outcomes by reducing fecal incontinence rates and supporting overall recovery:
-
Rehabilitation Techniques: Kegel exercises, biofeedback therapy, and electrical stimulation have been shown to reduce post-surgical fecal incontinence rates by 25-30%.5
-
Follow-Up Care: Regular follow-ups are crucial to monitoring the success of surgical repairs, detecting complications early, and adjusting rehabilitation protocols as needed.
Integrating pelvic floor rehabilitation, adjunctive therapies, and psychological support into the management of OASIs ensures a holistic approach, promoting both physical and emotional recovery.67
Colorectal Implications and Management of Obstetric Anal Sphincter Injuries (OASIs)
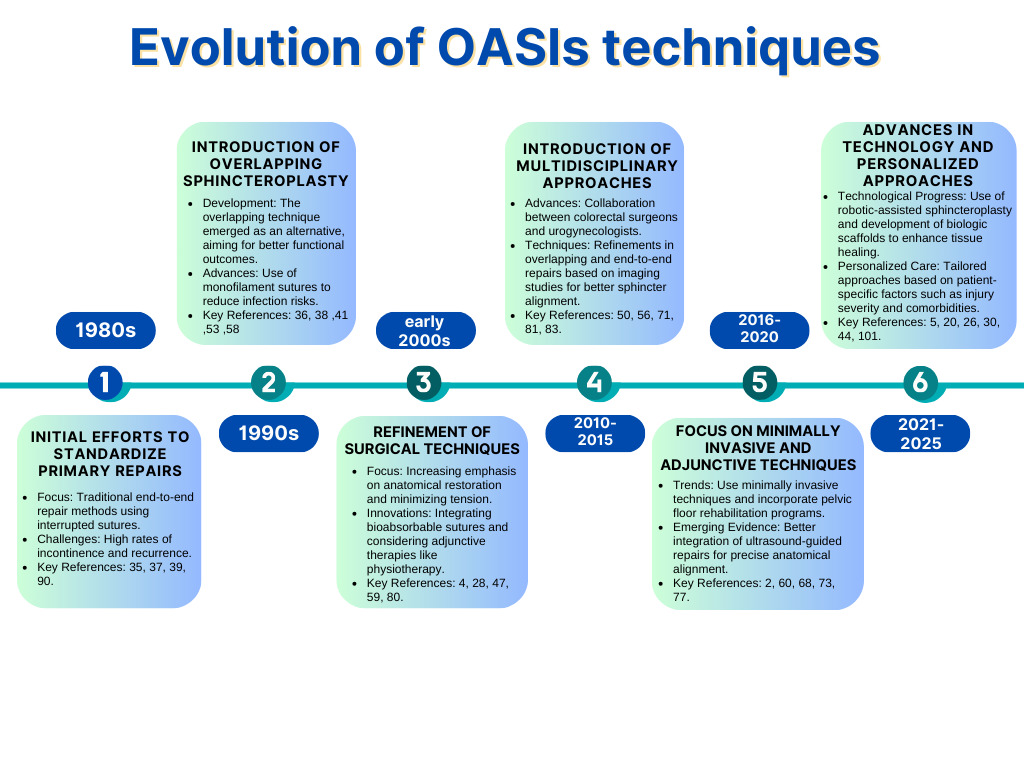
OASIs are a major public health issue with significant colorectal consequences. Disruption of the anal sphincter complex during childbirth can result in debilitating outcomes such as fecal incontinence, rectal urgency, and perianal pain, profoundly impacting the quality of life of affected women.31,38,92 OASIs surgical management has evolved over time, as shown in Figure 4. Beyond the immediate challenges of acute repair, these injuries have long-term implications for anorectal function, patient satisfaction, and healthcare systems.34,59,93 [Table 3].
Impact on Colorectal Function
OASIs frequently leads to both immediate and delayed colorectal dysfunction. Fecal incontinence is reported in 15%–61% of affected women, with anal urgency present in up to 45%.69,72,94 Chronic perineal pain and rectovaginal fistulas occur in 10%–20% of cases, especially following inadequate primary repair.5,33,44 These complications arise not only from mechanical sphincter disruption but also from pudendal nerve damage and pelvic floor dysfunction, which are often underappreciated in obstetric care.26,62,85
Advanced diagnostic tools, including endoanal ultrasound and manometry, are essential for detecting residual sphincter defects and dysfunction. Up to 70% of women show persistent sphincter defects post-repair, underscoring the importance of specialized colorectal follow-up for optimizing long-term outcomes.6,7,61,95
Role of Secondary Overlapping Sphincteroplasty
Secondary overlapping sphincteroplasty is the cornerstone surgical intervention for women with refractory fecal incontinence following OASIs [Figures 5-8]. The procedure restores anal canal structure and function by approximating the torn ends of the external anal sphincter with overlapping sutures.9,30,49 Collaboration between colorectal surgeons and gynecologists is often necessary to address the complex interplay of pelvic floor anatomy and function.41,63,91
Outcomes and Limitations
Symptomatic improvement following secondary sphincteroplasty is reported in 60%–80% of cases; however, objective metrics, such as anal pressures, often show limited gains.2,43,73 Furthermore, up to 50% of women experience recurrent symptoms within five years, emphasizing the need for careful patient selection and managing expectations.52,77,88 Postoperative fecal urgency affects 20%–40% of patients, highlighting the challenge of balancing continence and urgency.1,10,92
Timing and Challenges
Timing is critical in secondary sphincteroplasty. Early intervention, ideally within six months to one year, often achieves better outcomes, while delayed repairs are complicated by fibrosis, scarring, and potential pudendal nerve damage.35,47,57 Additional complexities arise in cases involving concurrent pelvic organ prolapse, rectocele, or enterocele, which may necessitate combined surgical approaches.18,48,68
Patients with extensive internal and external sphincter damage often require adjunctive treatments. Options such as sacral nerve stimulation or injectable bulking agents can provide symptomatic relief when sphincteroplasty alone is insufficient.21,40,79 Preoperative evaluation and long-term surveillance are essential for managing associated complications like rectal prolapse or chronic constipation.20,37,96
Emerging Perspectives
Innovative approaches are advancing the management of OASIs-related injuries. Techniques such as 3D endoanal ultrasound enhance diagnostic precision, while biomaterial grafts and regenerative therapies promise to improve surgical outcomes.10,36,55 Additionally, multidisciplinary care involving colorectal surgeons, urogynecologists, and physiotherapists is becoming increasingly integral to optimizing functional outcomes and patient satisfaction.16,22,32
From a colorectal perspective, secondary overlapping sphincteroplasty remains a key procedure for managing OASIs-related fecal incontinence. However, its limitations—such as recurrent symptoms and fecal urgency—highlight the need for a tailored approach. Addressing structural and functional sequelae, combined with emerging technologies and a multidisciplinary framework, is essential for improving the quality of care and outcomes for women affected by OASIs.56,84,97
Patient Satisfaction and Quality of Life with OASIs and Overlapping Sphincteroplasty
OASIs significantly impact patient satisfaction and quality of life (QoL), with both physical and psychological sequelae that persist long after childbirth. Fecal incontinence (FI), anal pain, and urgency are common consequences, leading to social withdrawal, reduced intimate relationships, and mental health issues like anxiety and depression. Women with FI are three times more likely to experience depression compared to the general population.19,45,61 Psychological distress further diminishes overall postnatal satisfaction.6,54,77
Quality of Life Outcomes Post-OASIs
-
Fecal Incontinence: Affects up to 60% of women, severely impacting physical and emotional health.69,72,94
-
Social and Psychological Impact: Chronic pain, sexual dysfunction, and mental health challenges, such as depression, anxiety, and shame, often accompany unresolved symptoms.2,57,85
-
QoL and Emotional Health: Addressing mental health is crucial for improving postpartum care and satisfaction.32,56,60
Patient Satisfaction After Overlapping Sphincteroplasty
Overlapping sphincteroplasty, the primary surgical intervention for persistent symptoms, offers symptom relief, but satisfaction rates vary from 50% to 80%. Around 70%–80% of women report improvement within the first year, but long-term satisfaction declines as recurrent symptoms, including FI and urgency, affect 30%–50% of patients over 5–10 years.23,41,62 Realistic expectations and improved emotional/social well-being are key contributors to higher satisfaction.27,57,61
QoL Metrics Following Sphincteroplasty
Sphincteroplasty improves QoL in lifestyle adaptation and coping strategies, but residual symptoms like minor leakage or urgency can persist.17,34,73 Sexual dysfunction, especially dyspareunia and reduced satisfaction, remains a concern even after anatomic repair.37,90,96 Postoperative complications, such as wound dehiscence and anal stenosis, further affect QoL.10,39,53
Psychological and Social Dimensions
Psychosocial support significantly influences satisfaction and recovery. Multidisciplinary care, including counseling and physiotherapy, reduces stigma and isolation, enhancing patient outcomes.5,20,67 Lack of support correlates with lower satisfaction and higher distress.46,59,88
Colorectal Perspectives on Improving Satisfaction
Optimizing patient satisfaction involves precise surgical planning, preoperative evaluation, and long-term follow-up.18,47,48 Adjunctive treatments like sacral nerve stimulation and bulking agents can complement sphincteroplasty in complex cases.21,43,84 Innovations in regenerative medicine, including stem cell therapies, promise to improve outcomes.28,68,98
While overlapping sphincteroplasty effectively relieves many women’s symptoms, patient outcomes are influenced by symptom resolution, expectations, and psychosocial support. A multidisciplinary, patient-centered approach is essential for improving QoL and satisfaction post-OASIs.11,13,55
Future Directions in Managing Obstetric Anal Sphincter Injuries (OASIs)
The management of Obstetric Anal Sphincter Injuries (OASIs) is advancing through preventive strategies, surgical innovations, regenerative medicine, and personalized care. Emerging technologies and a focus on comprehensive rehabilitation are pivotal in improving long-term outcomes.
Prevention of OASIs
Prevention remains the cornerstone of OASIs management. Established techniques like perineal support and controlled delivery have proven effective in reducing severe perineal trauma.30,62,94 Ongoing research aims to enhance risk assessment tools and standardize training for diverse obstetric populations to minimize OASIs incidence.33,44,92
Innovations in Surgical Techniques
Advances in surgical methods are enhancing outcomes for complex and recurrent injuries:
-
Overlapping Sphincteroplasty remains the standard repair method, though newer techniques like anterior sphincteroplasty and muscle interposition are being explored to improve outcomes for challenging cases. These techniques address the 25% of patients who continue to experience incontinence after standard repairs.2,44,99
-
Minimally Invasive Approaches: Robotic-assisted surgery offers improved precision and reduced complication rates, while laparoscopic-assisted repairs minimize recovery time and wound-related complications.37,58
-
Nerve Stimulation Therapies: Sacral nerve stimulation (SNS) has demonstrated a success rate of 70%-90% in improving continence and quality of life, while posterior tibial nerve stimulation (PTNS) provides symptom relief in 60% of cases.8,24,41,67,69,100
-
Injectable Bulking Agents: These provide a minimally invasive option for persistent symptoms, with agents like autologous fat showing promise in restoring sphincter function.7,51,100
Regenerative Medicine
Regenerative therapies are emerging as a promising field for OASIs management:
-
Stem Cell Therapy: Mesenchymal stem cells (MSCs) demonstrate potential in regenerating sphincter muscle and improving continence. Optimizing delivery methods and combining therapies are priorities for future research.28,34,64,89
-
Bioengineered Scaffolds: These scaffolds provide structural support for tissue repair, offering less invasive alternatives to traditional surgical techniques.18,45,101
Personalized Treatment Approaches
Tailoring treatments based on patient-specific factors, such as injury severity, comorbidities, and psychosocial needs, enhances outcomes. Predictive tools using machine learning are being developed to better stratify patients and guide clinical decisions.5,23,32,78,96,102
Postoperative Rehabilitation
A multidisciplinary approach to rehabilitation is essential for sustained recovery:
-
Pelvic Floor Therapies: Techniques such as Kegel exercises, biofeedback, and electrical stimulation reduce fecal incontinence rates by 25% to 30% and strengthen sphincter function by 40% to 50%.5,86
-
Adjunctive Therapies: Topical glyceryl trinitrate accelerates wound healing by 20%, while low-level laser therapy promotes recovery.8,64,85,86,90
-
Psychological Support: Addressing the mental health impacts of OASIs, including anxiety and trauma, is critical for holistic care.8,20,28,91
Long-Term Research Priorities
Future research should focus on large, multicenter studies to assess the durability of interventions, recurrence rates, and patient-reported outcomes. These studies will provide insights into the comparative effectiveness of surgical and non-surgical treatments and help refine long-term management strategies.43,67,90
Addressing Psychosocial and Cultural Barriers
Equitable care requires addressing cultural stigma and improving access in underserved populations. Culturally sensitive education and broader availability of specialized care are essential for improving outcomes.3,46,59
Exploring Novel Therapies
Emerging technologies offer the potential to revolutionize OASIs management:
-
Gene Therapy: Tools like CRISPR promise to regenerate damaged tissue and restore function.8,13,103
-
Bioelectronic Devices: These devices provide targeted neuromodulation for symptom relief, offering a futuristic alternative to traditional treatments.1,61,65
A combination of preventive measures, surgical advancements, regenerative approaches, and personalized strategies will define the future of OASIs management. Continued investment in long-term research, equitable care, and innovative technologies is essential to improve outcomes and quality of life for affected women.66,68,104
While emerging therapies such as regenerative medicine, nerve stimulation, and minimally invasive surgical techniques show promise in improving outcomes for women with OASIs, their feasibility, cost-effectiveness, and long-term efficacy require further exploration. Many of these treatments, including mesenchymal stem cell therapy and bioengineered scaffolds, have demonstrated potential in early studies,28,34,64,89 but their clinical application remains limited by challenges in scalability, regulatory approval, and cost. The high cost of novel technologies like robotic-assisted surgery and bioelectronic devices1,37,58,61 may restrict widespread adoption, particularly in resource-limited settings, highlighting the need for comparative cost-effectiveness analyses against traditional interventions such as overlapping sphincteroplasty. Additionally, while nerve stimulation techniques such as SNS and PTNS have reported success rates of 60%-90% in improving continence and quality of life,8,24,41,67,69,100 long-term data on durability and patient adherence remain limited. There is also a need for multicenter trials assessing these interventions’ sustained benefits and recurrence rates over decades.43,67,90 Addressing these gaps will require large-scale studies that evaluate clinical efficacy and consider economic viability, patient-reported outcomes, and accessibility, ensuring that future advancements in OASIs management are both effective and widely implementable.
The Critical Role of Training in Reducing OASIs and Improving Surgical Outcomes
Proper training is essential for reducing obstetric anal sphincter injuries (OASIs) and enhancing surgical outcomes. Comprehensive education ensures better prevention, diagnosis, treatment, and long-term recovery.
Training in OASIs Prevention
Structured training programs focused on preventive techniques significantly reduce OASIs risk. Methods like controlled delivery and perineal protection (e.g., “hands-on” or “Ritgen’s”) reduce OASIs rates by 40%–60%.70,73,78 Ultrasound-guided training on episiotomy angles cuts severe tears by 30%,54,100 demonstrating the importance of integrating evidence-based strategies through regular training and audits.30,62,77
Accurate Diagnosis and Classification
Timely diagnosis of OASIs is crucial for effective management. Training in perineal injury classification using standardized guidelines (e.g., RCOG) improves diagnostic accuracy and reduces underdiagnosis.33,38,78 Regular feedback and audits refine providers’ diagnostic skills.57,58,85
Surgical Training in Overlapping Sphincteroplasty
Advanced training in overlapping sphincteroplasty improves outcomes, with continence restoration rates of up to 85% in trained providers, compared to 60% in less experienced surgeons.7,41,68,105 Simulation-based learning, cadaveric dissections, and competency-based assessments improve precision by 25% and reduce complications by 15%.55,56,89 Multidisciplinary collaboration enhances patient satisfaction, with rates exceeding 90%6,50,58
Impact of Training on Patient Outcomes
Trained providers achieve better functional and psychosocial outcomes. Advanced surgical techniques improve continence and quality of life, while patient-centered communication enhances recovery and expectation management.5,28,59,64,84,86
Use of Technology in Training
Technological innovations, including VR and AI-driven platforms, offer risk-free practice and real-time feedback, enhancing decision-making and technical skills.71,89,96
Sustained Education and Skill Maintenance
Ongoing education, including CPD programs and mentorship, is vital for maintaining proficiency.49,67,90 Structured mentorship ensures less experienced providers gain essential skills.20,46,66
Improved Patient Outcomes
Investing in provider training reduces complications, recurrence rates, and patient dissatisfaction. Women treated by trained professionals report better symptom resolution and quality of life.2,65,99
Comprehensive training in OASIs prevention, diagnosis, and management improves patient outcomes. Standardized training, technological innovations, and interdisciplinary collaboration ensure better care and long-term recovery.1,68,82 Investing in education is crucial to advancing OASIs management and addressing its multifaceted challenges.
Research gaps
Despite advances in the prevention and management of OASIs, significant gaps remain in current research and clinical practice. One major limitation is the variability in long-term outcomes following overlapping sphincteroplasty, with studies reporting recurrence rates of fecal incontinence ranging from 30% to 50% over 5–10 years.23,41,62 This raises questions about the durability of surgical repairs and highlights the need for standardized long-term follow-up protocols. Additionally, while sacral nerve stimulation (SNS) and posterior tibial nerve stimulation (PTNS) have shown success rates of 60%–90% in managing refractory fecal incontinence,8,24,41,67,69,100 there is limited research on patient selection criteria, long-term efficacy, and cost-effectiveness, warranting further investigation. Another critical gap is the limited exploration of regenerative therapies, such as stem cell treatments and bioengineered scaffolds, which have shown promise in early studies but lack large-scale, multicenter trials to confirm their safety, feasibility, and clinical efficacy.28,34,64,89,101 Similarly, while machine learning and predictive tools are being developed to personalize treatment approaches,5,23,32,78,96,102 their integration into clinical practice remains in its infancy. Moreover, research on the psychosocial impact of OASIs remains underdeveloped, with many studies focusing on physical outcomes rather than the broader quality-of-life implications, including mental health, social reintegration, and sexual function.2,57,85 Addressing these research gaps through robust, longitudinal studies will be crucial in refining treatment protocols, optimizing patient-centered care, and developing innovative therapies to enhance long-term outcomes for women affected by OASIs.
Limitations
This systematic review has several limitations that must be considered when interpreting its findings:
-
Heterogeneity of Evidence: The available literature on OASIs exhibits significant variation in study design, patient demographics, surgical approaches, and outcome measures. This variability limits the ability to derive consistent conclusions or establish standardized management protocols.
-
Limited Long-Term Follow-Up: While many studies provide valuable insights into short-term outcomes, there is a lack of robust long-term data on the durability of interventions, particularly for secondary overlapping sphincteroplasty and emerging therapies.
-
Inconsistent Reporting Standards: Variability in the classification of OASIs, documentation of surgical techniques, and descriptions of postoperative care across studies impede direct comparisons and complicate the formulation of universal treatment recommendations.
-
Publication Bias: The predominance of studies reporting positive outcomes raises concerns about publication bias, potentially overestimating the success of interventions while underrepresenting complications, failures, or negative outcomes.
-
Scarcity of Evidence on Adjunctive Therapies: While rehabilitation programs, biofeedback, and psychological support are integral to recovery, there is limited high-quality evidence evaluating their efficacy when used alongside surgical interventions, leaving gaps in understanding comprehensive care strategies.
-
Geographic and Resource Disparities: Most studies originate from high-income settings, which may not be generalizable to low-resource environments where access to specialized care and expertise in managing OASIs is often limited. This creates a gap in understanding global applicability.
-
Subjectivity in Outcome Measures: Reliance on patient-reported outcomes for continence, quality of life, and satisfaction introduces subjectivity and variability. While valuable, these outcomes are influenced by individual perceptions and may not fully capture objective measures of success.
By acknowledging these limitations, this review underscores the need for further research to address these gaps and advance the understanding and management of obstetric anal sphincter injuries.
Conclusions
-
Impact of OASIs: Obstetric anal sphincter injuries (OASIs) remain a significant maternal health challenge, causing long-term complications such as fecal incontinence, chronic pain, and psychological distress. These injuries profoundly affect women’s quality of life and necessitate holistic management approaches.
-
Surgical Interventions: Secondary overlapping sphincteroplasty effectively treats symptomatic OASIs, providing significant short-term symptom relief. However, its long-term efficacy diminishes over time, with the recurrence of incontinence reported in many cases. Emerging techniques, including robotic-assisted procedures and regenerative therapies, show promise in addressing these limitations.
-
Adjunctive Therapies: Non-surgical interventions, such as sacral nerve stimulation (SNS), posterior tibial nerve stimulation (PTNS), and biofeedback, offer effective symptom management for refractory cases. These therapies and pelvic floor rehabilitation improve functional outcomes and quality of life.
-
Multidisciplinary Care: Individualized management, incorporating risk factor modification, tailored surgical techniques, and comprehensive rehabilitation, is essential for optimizing outcomes. Addressing the psychological and social impacts of OASIs is also critical to ensuring holistic care.
-
Future Directions: High-quality, multicenter studies are needed to evaluate the long-term durability, cost-effectiveness, and patient-reported outcomes of existing and emerging therapies. Advances in regenerative medicine and predictive tools hold potential for transforming OASI management.
Recommendations
-
Focus on Prevention: Obstetric practices should prioritize prevention strategies, such as perineal support during delivery and standardized training for obstetric teams, to minimize the incidence of OASIs.
-
Refinement of Surgical Techniques: Research into novel surgical techniques, such as robotic-assisted sphincteroplasty and muscle interposition, should be prioritized to improve long-term outcomes, particularly in recurrent or complex cases.
-
Integration of Adjunctive Therapies: Adjunctive treatments, such as sacral nerve stimulation and regenerative approaches, should be incorporated into clinical practice for cases where surgical repair alone is insufficient. Future studies should establish standardized protocols for these therapies.
-
Comprehensive Rehabilitation: Postoperative care should include structured rehabilitation programs combining pelvic floor physiotherapy, biofeedback, and mental health support to optimize recovery and address psychosocial impacts.
-
Research and Innovation: Investments in regenerative medicine, such as stem cell therapy and bioengineered scaffolds, are needed to develop minimally invasive alternatives for OASI repair. Predictive machine learning tools should be explored to personalize care and stratify patients based on risk and severity.
-
Education and Awareness: Culturally sensitive education initiatives and efforts to address stigma surrounding childbirth injuries are essential to improving access to care and patient outcomes, particularly in underserved populations.
-
Long-Term Follow-Up: Establishing long-term follow-up programs to monitor recurrence rates, complications, and patient-reported outcomes is essential to understanding the durability of current and emerging interventions.
By combining prevention, innovative treatments, and holistic care, the management of OASIs can be significantly enhanced, ultimately improving the quality of life for affected women.