Introduction
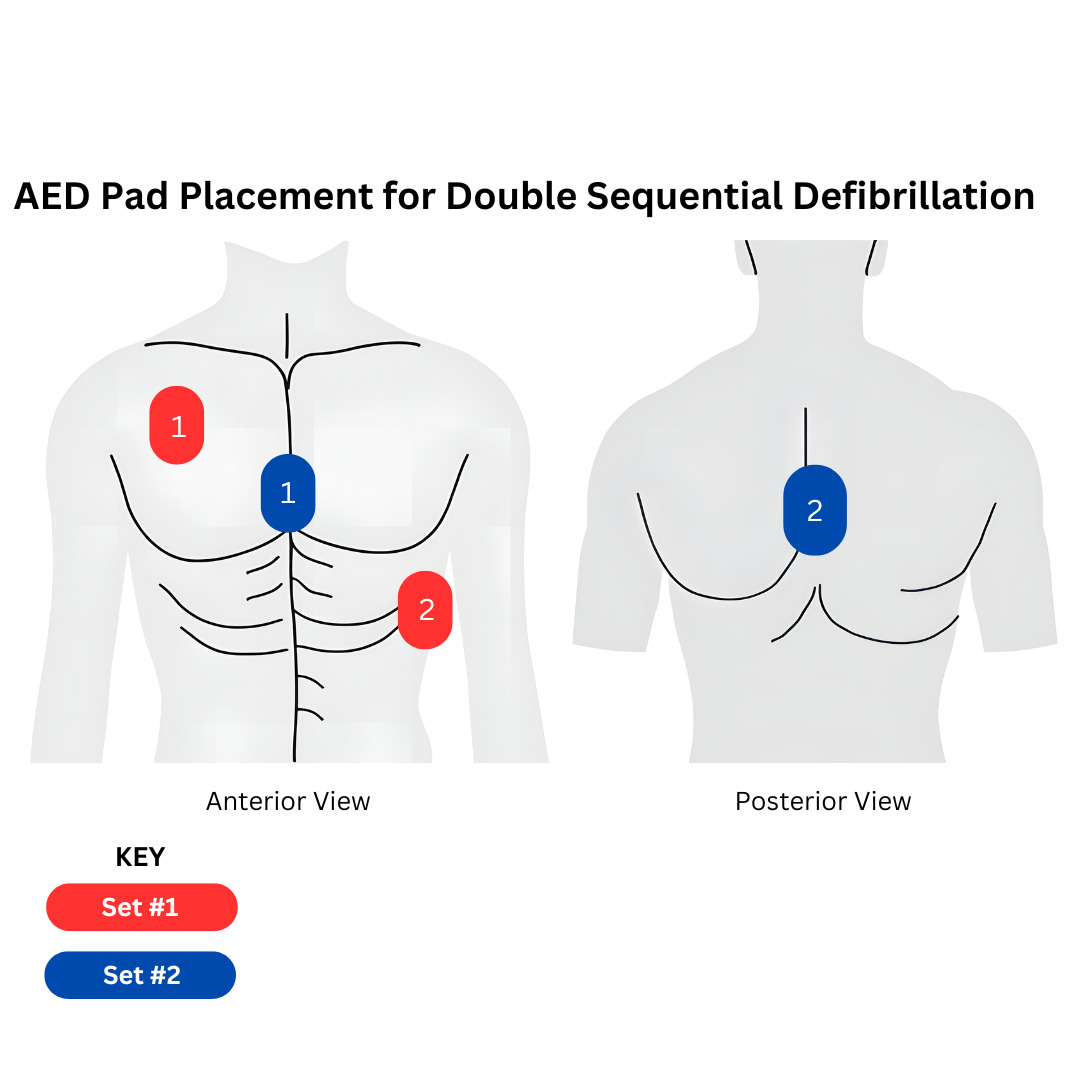
Cardiac arrest secondary to ventricular fibrillation is treated with defibrillation, placing one set of defibrillator pads on the patient’s chest and shocking them.1 Ventricular fibrillation is a shockable cardiac arrest rhythm responsible for high mortality rates. Every year, an average of 814,000 patients in the United States and Europe are treated for cardiac arrest, and out of these people, 163,000 have a recorded rhythm of ventricular fibrillation.2 On average, survival after ventricular fibrillation is associated with CPR initiated in 13 minutes or less and defibrillation occurring in 23 minutes or less.3 The objective of this study is to describe the outcomes of prehospital double sequential defibrillation on refractory ventricular fibrillation. Double sequential defibrillation (DSD) involves two sets of defibrillators rather than one, with placement of one set of pads in standard defibrillation position, and the other set of pads on the front and back of the chest area [Figure 1].4 DSD is controversial, and opinions among medical practitioners are divided, due to the lack of research behind it.5 DSD has been proposed as a treatment for a certain state of ventricular fibrillation that occurs when it does not convert after three shocks of standard defibrillation, termed refractory ventricular fibrillation.
Methods
This analysis is sourced from Polk County Fire Rescue’s EMS prehospital IRB-approved research registry, as part of the Cardiac Arrest Registry to Enhance Survival (CARES) database. The Polk County Fire Rescue system, encompassing more than 2010 square miles, is one of the largest in the state of Florida. This dataset includes all refractory ventricular fibrillation patients in the county who underwent double sequential defibrillation over a 24-month period. In total, 29 cases fulfilled the requirements for refractory ventricular fibrillation. Return of Spontaneous Circulation (ROSC) refers to patients who had a palpable pulse for 30 seconds or more.
Results
The cohort contained a total of 29 cases. The second set of pads required for double sequential defibrillation was positioned in the antero-postero direction, while the first set was positioned in the standard anterior-lateral direction. Both sets of defibrillators had an applied energy level of 200J. The shock-to-shock cycle time was less than 20 seconds. Fifteen cases occurred in year 1, while 14 cases occurred in year 2. Approximately 28.6% of the patients in year 2 (4 individuals) achieved a return of spontaneous circulation, whereas only 20% of the cases in year 1 (3 individuals) achieved ROSC in year 1. The percentage of survival to hospital discharge of patients who achieved ROSC was 100% (4 individuals) in year 2, whereas 66% (2 individuals) of ROSC patients survived to hospital discharge in year 1. The overall percentage survival to hospital discharge of all refractory ventricular fibrillation patients was 13.3% in year 1, and 28.6% in year 2 (Figure 1).
When looking at both years in total, approximately 24.1% (seven individuals) achieved a return of spontaneous circulation after going through double sequential defibrillation, while 20.7% (6 individuals) of all refractory ventricular fibrillation patients shocked with double sequential defibrillation survived up to hospital discharge. In both years, 85.7% (6 patients) of all patients who achieved ROSC survived up to hospital discharge.
Discussion
According to the American Heart Association, “The usefulness of double sequential defibrillation for refractory shockable rhythm has not been established.” It is currently not recommended.6 Additionally, current studies on DSD are not clearly defined and yield varying results, despite the popularity of DSD as a treatment increasing.7 However, it is often still used in situations when nothing else can be done, and there have been many studies investigating whether DSD can be used when standard defibrillation does not work.
A 2020 study found no difference when DSD was used in neurologic outcome, hospital discharge time, ROSC, or any improvement in return of spontaneous circulation when compared with traditional defibrillation.8 Another study from 2020 showed a rate of 40% ROSC in patients treated with DSD, compared to a 25% ROSC in patients treated with standard defibrillation. DSD also yielded a rate of 76.3% ventricular fibrillation termination, compared to a 66.6% rate in patients treated with standard defibrillation.9 The study concluded that this new treatment is feasible and safe when there are no other options, and the current study reflects this.
A case study documented a 51-year-old patient who had come to the emergency department with ventricular fibrillation. There was no response after 10 rounds of standard defibrillation. However, after two rounds of DSD, the patient achieved ROSC and survived to hospital discharge.10
Another study supported the claim that there is no evidence to show that DSD is feasible for ventricular fibrillation. However, the review shows that those who received DSD survive better to discharge. However, there are other factors impacting this, such as the number of standard shocks received before DSD was administered.11
A 2023 study showed a slight increase in the number of patients surviving to hospital discharge when treated with DSD compared to those patients who were treated with traditional single defibrillator defibrillation.12 30.4% of patients with DSD in this study survived to hospital discharge, while patients treated with standard defibrillation only had a 13.3% survival rate. This study also demonstrated a higher rate of ROSC when DSD was used on ventricular fibrillation patients. Another 2023 study supporting DSD showed that DSD can successfully terminate VF in cases where CPR and standard defibrillation are not working. After six standard shocks, ROSC was initially achieved, but the patient went back into refractory ventricular fibrillation recurrently, which caused the physicians to turn to DSD, which was successful.13
There are proposed theories in past studies as to why DSD and DED (double external defibrillation), in some cases, causes improved ventricular fibrillation patient outcomes. One theory is that the administration of more joules of shock, causes the myocytes in the heart to convert quicker and easier. This theory is dubbed the Power Theory, and from this study, it seems to show that DSD can be effective in administering more joules of shock. The study also discussed another theory as to why DSD has positive outcomes in some cases, which is regarding the two shocks administered to the patient in DSD. This theory says that the first shock lowers the defibrillation threshold or the number of joules required for the myocytes to convert, thus the second shock is effective in converting any remaining fibrillating myocytes. This theory states that in standard defibrillation, in some cases, only some, not all, of the myocytes are converted, which is why the patient does not achieve ROSC in those cases. Thus, the study concludes that in those specific cases where myocytes are not converted after the first shock, DSD can be useful in administering a second shock to ensure all myocytes are converted. This is dubbed the Setting Up theory.14
These theories can apply to the results in the above section. The slightly increased number of patients administered DSD could have been those cases where all of the myocytes were not converted with standard defibrillation, thus DSD was needed. However, it is critical to mention this method is not foolproof, and not necessarily every single patient will see improvement due to DSD. There is no proper causational relationship between DSD and patient outcomes, but there are explanations and theories as to why it does cause improved outcomes in some patients. While these theories do not seem to apply to every single patient, from the results above and the results of the studies investigated, it seems that there are certain cases in which DSD can successfully apply any of these theories to result in a positive ROSC outcome for patients with ventricular fibrillation.
Conclusion
For patients who experience ventricular fibrillation that did not convert after three shocks, a valid treatment option could be to implement double sequential defibrillation with two sets of defibrillators rather than one. Rather than letting someone with refractory ventricular fibrillation die, double sequential defibrillation is a treatment option that is effective in some cases, which is why it should be considered an option for refractory ventricular fibrillation patients.