Introduction
Angioedema is a localized, paroxysmal, non-pruritic, non-pitting swelling of the subcutaneous tissue or submucosa.1 It typically affects areas with loose connective tissue, such as the face, lips, tongue, uvula, larynx, and can even affect the bowel wall. Angioedema can be mediated by mast cells (also known as histaminergic angioedema), by bradykinin, or by other unknown etiologies. Unlike mast cell-mediated angioedema, bradykinin-induced angioedema is not associated with other symptoms of allergic reactions such as urticaria, bronchospasm or hypotension.2
A common cause of bradykinin-mediated angioedema is angiotensin-converting enzyme inhibitors (ACE-Is). Nearly half of the adults in the United States have hypertension, and 4 in 5 of those adults (94.9 million) are recommended by a clinician to take prescription medication(s) to treat their hypertension.3 ACE-Is are one of those medications, and according to the National Health and Nutrition Examination Surveys (NHANES), the ACE-I lisinopril was the most commonly used antihypertensive drug in the United States by 2010, with 20.1% of the hypertensive population taking lisinopril.4 Nonetheless, the incidence of angioedema in patients taking ACE-Is is low, with 1 to 7 cases reported per 1000 patients in most studies, although the risk is 4.5 times higher for black Americans.5 ACE-I-induced angioedema accounts for up to one-third of all emergency department visits for angioedema because of the prevalence of their use in the practice of medicine.1
However, angioedema is not the only cause of facial swelling. The differential diagnosis of facial swelling is vast: allergic reactions due to foods, medications, insect bites, or various environmental allergens; infections such as sinus infections, dental infections, or cellulitis; trauma such as a broken nose or other injuries; or medical conditions such as Cushing’s syndrome or superior vena cava syndrome (SVCS).
Case
We present a case of a 61-year old African-American male who presented to the emergency department with the chief concern of facial swelling. Upon initial evaluation, the patient reported left-sided lower lip swelling which began the previous night. He reported awakening that morning with swelling across the lower half of his face, as pictured in Figure 1, which prompted him to present to the emergency department for evaluation. He denied difficulty breathing. The patient endorsed a history of hypertension, but he could not recall what medications he had been prescribed. We subsequently contacted the patient’s sister who informed us that the patient was taking lisinopril. The patient also reported this facial swelling had occurred once before, approximately a month ago, but had self-resolved so he did not seek medical care at that time. He had been given 50 mg of diphenhydramine intravenously by pre-hospital workers prior to arrival without any relief. At this point of the evaluation, suspicion for lisinopril-associated angioedema was high and our clinical plan was to stop that medication and monitor the patient to ensure that his swelling did not worsen. The swelling was mild and did not involve his tongue or posterior pharynx.
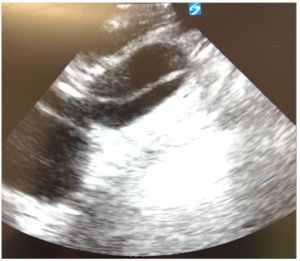
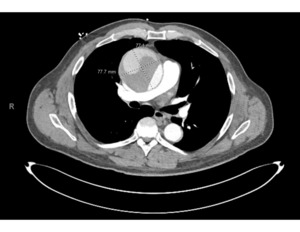
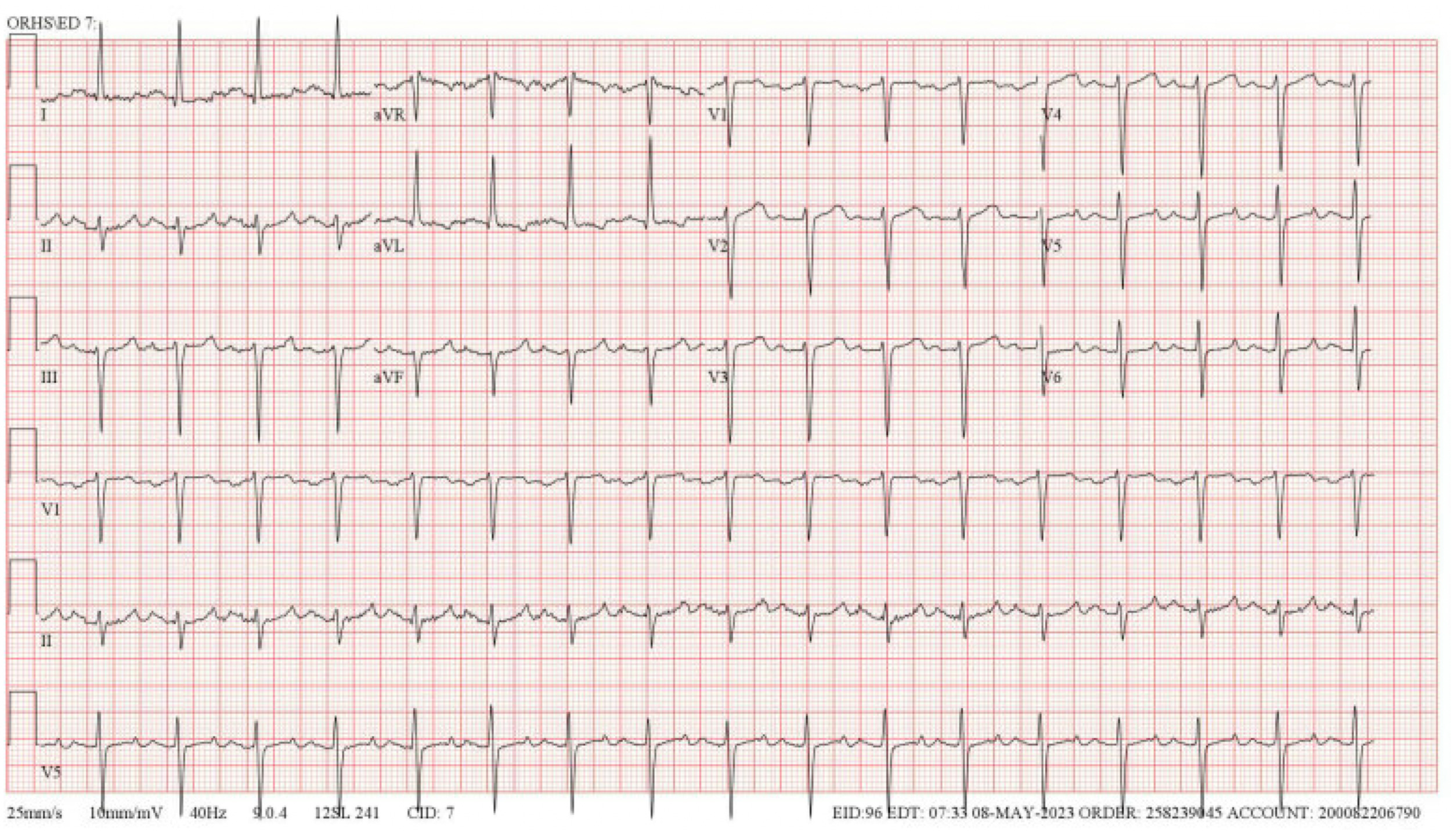
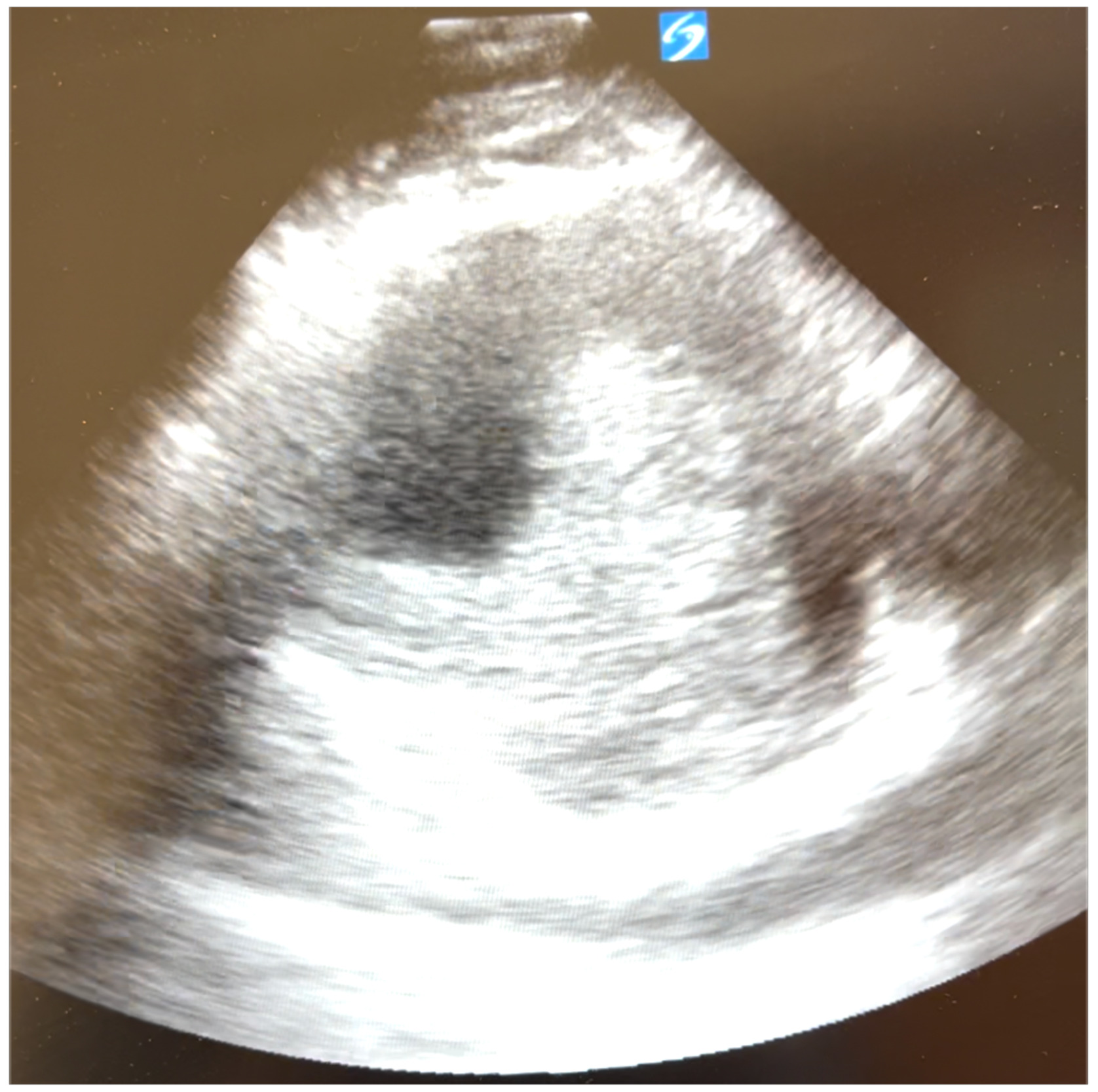
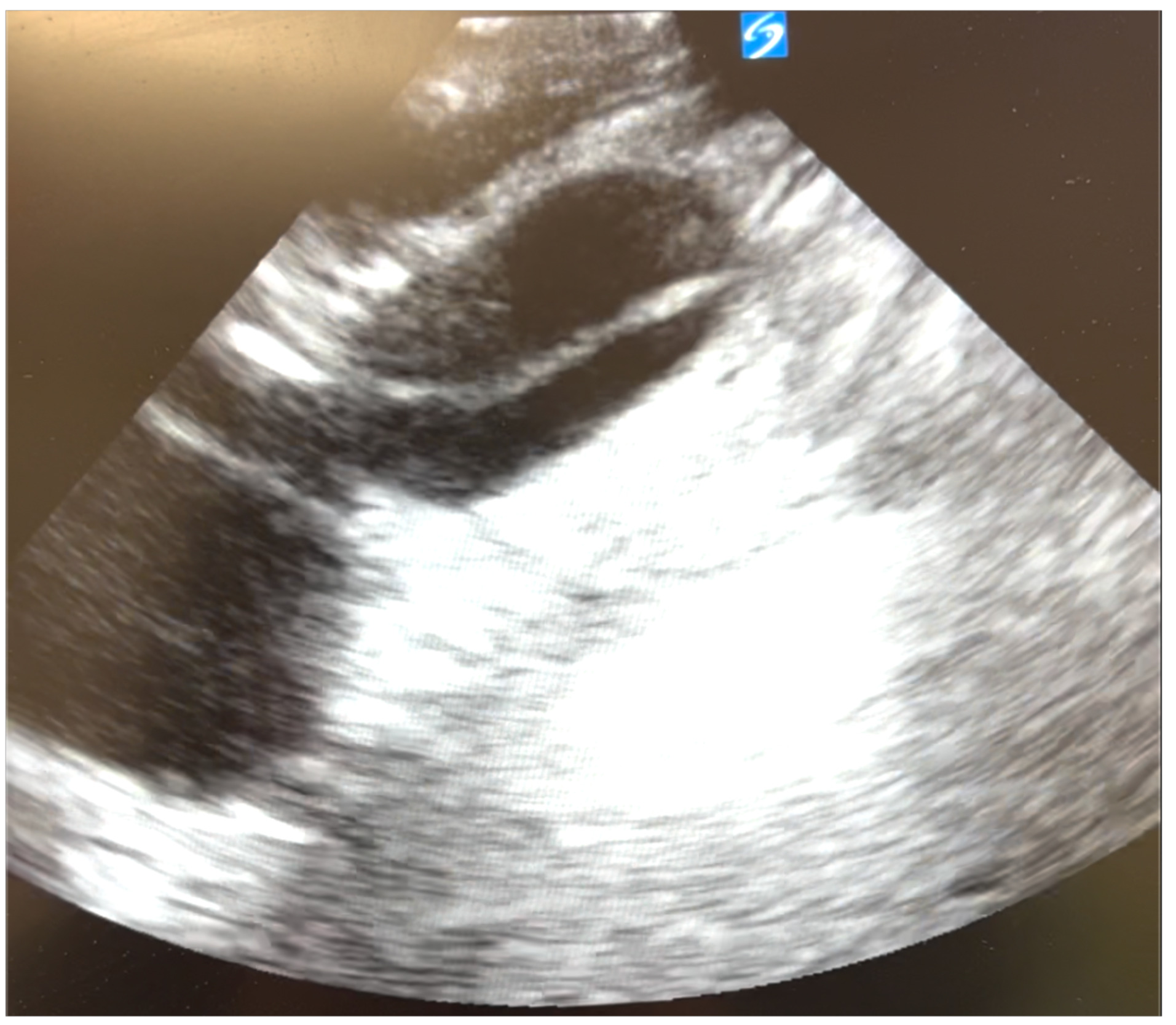
However, upon further careful medical history taking, the patient also reported chest pain that started that morning. He stated that the pain was located over the left side of his chest, felt sharp, was intermittent, but not worsened with exertion. He denied any recent upper respiratory infection, trauma to the chest, history of drug use, or previous history of chest pain.6 Although his blood pressure and heart rate were mildly elevated, his cardiac examination was normal, and he had good pulses in all of his extremities. We ordered tests to assess for potential acute coronary syndrome including electrocardiograms (ECG), high sensitivity troponins, and chest radiography. The ECG (Figure 2) showed sinus tachycardia at about 102 beats per minute, poor R wave progression across the precordial leads suggestive in this case of previous anteroseptal injury, and left ventricular hypertrophy per the modified Cornell criteria, but no ST segment elevations concerning for acute cardiac ischemia. The high-sensitivity troponin was very minimally elevated to 0.07 and downtrended to 0.06 three hours later. All other labs were grossly unremarkable besides mildly elevated liver function tests. The portable chest radiograph, however, showed a modestly widened superior mediastinum, as pictured in Figure 3. We quickly proceeded with a bedside ultrasound which showed a large ascending aortic aneurysm (Figure 4) with an associated proximal aortic dissection. In Figure 5, a dissection flap can be clearly visualized. After consulting with cardiothoracic surgery while starting the patient on an esmolol drip for blood pressure and impulse control, we obtained a CT angiogram of the chest which showed a 7.7 cm dissecting aneurysm involving the ascending aorta and proximal aortic arch with a large, partially thrombosed false lumen and extension into the proximal innominate artery (Figure 6). The radiologist also noted there was marked compression of the superior vena cava (SVC) due to the large aneurysm of the ascending aorta. The patient later required a nicardipine drip after high-dose esmolol failed to optimally control his hyperdynamic state.
The patient was taken emergently to the operating arena where a 6.5-hour complex operation ensued. The patient was placed on cardiac bypass, a diseased ascending aorta into the mid-arch was resected and grafted successfully with a large amount of thrombus removed. The patient was transferred to the cardiovascular recovery suite in stable condition and was extubated the next day. He was re-intubated soon after extubation. This was followed by a stormy post-surgical course and prolonged ICU stay with multiple complications, including a hemothorax, a pulmonary embolism, a retroperitoneal hematoma, and SVCS. Life support was terminated after an intensive five-week hospital stay.
Discussion
The suspected angioedema that our patient presented with was likely facial swelling from SVCS caused by the ascending aortic aneurysm. Although ACE-I-mediated angioedema in our patient on lisinopril seemed like the obvious cause of his facial swelling, the swelling continued to worsen during the patient’s stay in the intensive care unit, despite discontinuation of lisinopril.
The CT scan prior to surgery had shown marked compression of the SVC from the ascending aortic aneurysm. Despite significant thrombus removal, a large postoperative hematoma remained surrounding the area of dissection repair, which continued to compress the SVC, thus causing SVCS.
Superior vena cava syndrome is most commonly caused by advanced stages of lung cancer and non-Hodgkin’s lymphoma.7,8 In the mid-20th century, mediastinitis caused by tuberculosis and syphilis were the dominant causes of non-malignant SVCS.7 Today, only 5% to 22% of all cases of SVCS in developed countries are not caused by cancer, and most of these are caused by thrombosis due to central venous catheters and pacemakers.7
Thoracic aortic aneurysm, which itself is reported to have a prevalence of 0.16%, is a rare cause of SVCS, with only a few previously documented cases.9 In our case, the SVC was likely gradually compressed and obstructed by enlargement of the ascending aorta. In cases like this, in which the obstruction of the SVC has a slow mechanism and is incomplete, patients may remain asymptomatic for a long period of time as a network of collateral blood vessels grows, as likely happened in our patient.10,11 Even if our patient was symptomatic, the clinical signs of SVCS are often very nonspecific, ranging from simple facial and/or upper extremity swelling, often with headaches due to increased intracranial pressure, all the way up to hypotension and syncope. Especially in nonmalignant cases of SVCS, all of these factors can misdirect the correct diagnosis, as it did for us. Thus, it is important to keep the differential diagnosis broad, even when the diagnosis seems obvious.