Case Summary
A 25-year-old mentally retarded male patient admitted to a surgical casualty ward with 1 week history of abdominal pain and distension which was associated with failure to pass feces and flatus, last 3 days he had feculent vomiting and on the day of admission, he had spontaneous fecal discharge from right inguinal region. Up on further questioning, he was seen by a local doctor and prescribed some analgesics and phosphate enema. He denies any remarkable clinical improvement. He has no other comorbidities and rest of the history was unremarkable.
On examination he was ill looking and dehydrated with pulse rate of 110 beats per minute, blood pressure of 80/50 mmHg. He was febrile and running the temperature of 40 degree Celsius. Abdominal examination revealed distended, tympanic and non-tender abdomen in all four quadrants. He had a hard swelling in right inguinal region with a discharging sinus containing small bowel contents. In digital rectal examination, rectum was empty and otherwise he was mentally sound. His chest examination was unremarkable.
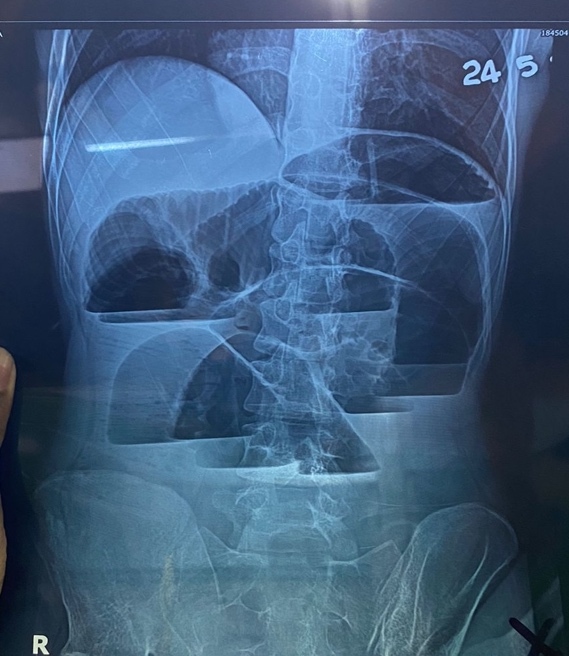
He was resuscitated with 1 l of normal saline and blood sample taken for basic investigation. He had urinary catheter and nasogastric tube placed in the casualty ward. After consultation with Microbiologist as per local guideline broad-spectrum IVAB stared following blood culture. The full blood count showed significant leukocytosis of 18,000 with predominance neutrophilia and CRP of 314 mg/dl. Abdominal X-ray erect film showed dilated small bowel loop with multiple air-fluid levels and no pneumoperitoneum.
The patient and family members were informed about the need for immediate laparotomy and got the consent for stoma as well. We approached the abdomen through midline incision after isolating bilateral groin area. Intraoperative findings were remarkable for significantly dilated small bowel with herniated segment of terminal ileum, 20cm from ileocecal valve into right groin deep ring. Also, there were multiple small bowel perforations proximal to the site of obstruction with significant fecal spillage. We disconnected herniated bowel loop from the deep ring and applied proximal and distal soft bowel clamps to control intestinal spillage as it was necrotic in the inguinal canal. The peritoneal cavity thoroughly washed with plenty of warmed normal saline until no food residue remains.
Since the patient was sick and hemodynamically unstable, we decided to perform small bowel resection and exteriorize proximal end as end ileostomy and distal end as mucus fistula. The groin deep ring was closed internally with 2/0 Polypropylene purse string suture and unhealthy inguinal skin edges trimmed and dressing applied. He was managed in Intensive care unit with dual antibiotics and analgesics, his recovery was slow and uneventful. On postop D5, inguinal wound closed and patient was discharged on D8.
He had clinic review in 2 weeks, midline incision was healed was histology was studied. He underwent 2nd laparotomy in 6 weeks to reestablish the continuity of intestine.
Introduction
A hernia is defined as the protrusion of part or whole of viscus through the wall of the cavity that normally contains it. Inguinal herniae involve abdominal contents passing into the inguinal canal and can continue into the scrotum as well. The groin hernias account for about 75% of ventral hernias. Most of the inguinal hernias asymptomatic and doesn’t warrant intervention. In general, we offer surgery for all symptomatic hernias and asymptomatic hernias where future chances of having complication is detrimental.
Richter’s hernia is a special and uncommon type of hernia where only a part of antimesenteric bowel wall is incarcerated within the hernia sac results in ischemia, gangrene and perforation of hollow viscus.1 It is commonly described in femoral hernia but rarely may present in inguinal hernia as well. Lack of awareness about this condition being the commonest reason for delayed diagnosis and increased morbidity.2
The most feared and fatal complication of hernia is bowel strangulation. Here, we report a case of strangulated bowel presenting with spontaneous fecal fistula due to either negligence or lack of awareness.3 Another downside of delayed diagnosis especially in adult male is testicular gangrene due to compromised cord vessels.2
Discussion
The delayed diagnosis of strangulated hernia can actually transform a benign condition to highly morbid condition. Both patient and health care play a role in undue delay. Ignorance, lack of awareness, doctor shopping and fear of surgeries are the common reasons from patient’s side and incorrect diagnosis, unavailability of image and surgical facilities being the reason from healthcare side for the delayed intervention. The unnecessary delay in diagnosis and treatment result in various complications like Necrotizing fasciitis, gangrenous testis and spontaneous fecal fistula.2,4 This emphasizes the need for health education and public awareness to avoid crippling complications.
Necrotizing fasciitis is a surgical emergency which require early resuscitation and debridement. In this scenario, perforated bowel being the source of microorganism. The progression of infection depends on the host immunocompetency and virulence of microorganism. Due to nonspecific clinical manifestations, serial clinical examination utmost important for the early diagnosis. Fortunately, our patient recovered from sepsis with a single debridement due to early intervention and limited nature of infection.
None of the sophisticated investigations can replace the clinical examination. Importance of looking at hernial orifices as a part of abdominal examination is very well pointed out in my patient. Routine examination of hernia offices can avoid a case of negligence. Especially, my patient being a mentally retarded he is potential candidate for negligence and delayed diagnosis due to unreliable symptomatology.
The uncommon but important Richter’s hernia is sometime misleading due to lack of obstructive symptoms. Since the pathology is only involves part of bowel circumference, typical bowel obstruction features like vomiting, absolute constipation and abdominal distention are minimal. The learning point here is that bowel obstruction cannot be excluded just by the lack of typical symptoms.
There is no definitive answer in literature as to how to approach complex perforated hernia with necrotizing fasciitis. Firstly, we addressed the abdominal pathology through midline laparotomy with segmental small bowel resection without abdominal contamination and simultaneously closed the deep ring internally. Secondly, we did wound debridement which significantly minimize the wound contamination.
Our patient had significantly dilated small bowel with perforation leading to minimal peritoneal spillage and his physiology is not favorable to do primary anastomosis. So, we created proximal end as end ileostomy and distal end as mucus fistula. The stoma is lifesaving especially in acutely ill patients.
This case report reiterates the importance of having high suspicion of Richter’s hernia even in the absence of obstructive symptoms and it requires early diagnosis and prompt treatment.
Learning Points
-
Always ensure to examine hernial orifices as a part of routine abdominal examination in order to avoid medical negligence.
-
The Richter’s hernia can present with lack or absence of obstructive bowel symptoms.
-
Delayed presentation of strangulated inguinal hernia can complicate with testicular gangrene, necrotizing fasciitis and spontaneous fecal fistula.